INTRODUCTION
In the United States, type 1 diabetes mellitus (DM) is diagnosed in approximately one in every 300 individuals under the age of 18 years [1]. The prevalence ranges from 5.4 to 79.6 cases per 100,000 population [2]. It is estimated that 15% to 20% of type 1 DM cases in children occur during preschool age, specifically under the age of 6 years [3]. The prevalence of this disease in preschoolers has been increasing annually, reaching 5.4% in 2017 [4]. The global incidence of type 1 diabetes in children is on the rise, largely due to the recent increase in obesity rates [5]. In Korea, the prevalence of type 1 DM in children and adolescents has increased from 3.70 per 100,000 individuals in 2008 to 4.77 in 2016, constituting an annual increase of 3% to 4% [6]. DM is the most common chronic disease in childhood [7] and is caused by either abnormal insulin secretion from the pancreas or ineffective utilization of the insulin produced [8]. Type 1 DM, which primarily occurs in childhood, results from the destruction of pancreatic beta cells by T cells of the immune system [9]. This condition necessitates invasive insulin treatment to regulate blood glucose levels [8]. Maintaining appropriate glucose levels in preschool children is crucial for their growth and development and for preventing complications [10].
During the preschool years, type 1 DM adversely impacts a child's overall lifestyle and development, affecting play, sleep, eating patterns, and relationships with family and others [3]. It is essential to manage and control blood glucose levels at this time, as poorly managed diabetes can result in serious complications such as seizures, coma, diabetic ketoacidosis, nephropathy, and neuropathy [11]. However, diagnosing and managing type 1 DM in preschool-aged children presents unique challenges, as it requires consideration of the child's developmental characteristics from both medical and psychosocial standpoints [12]. For instance, preschoolers are highly sensitive to insulin and are at increased risk of nighttime hypoglycemia due to high fluctuations in blood glucose levels caused by rapid physical development [13]. Furthermore, consuming enough food and maintaining a balanced diet can be difficult, as children at this developmental stage often exhibit temporary food preferences or aversions [14].
Preschoolers undergo a period of rapid physical and neurological growth, making it crucial to monitor and regulate their blood glucose levels to prevent hypoglycemia [15]. Moreover, fluctuations in blood glucose during this stage can have a more detrimental impact on brain development than at other ages, leading to a decrease in overall cognitive function in children [15]. The cognitive and linguistic immaturity of preschoolers, coupled with the often asymptomatic nature of diabetes at this age, makes it challenging for parents to recognize and identify symptoms of hypoglycemia in their children. This can result in parental fears related to hypoglycemia in children [13,16].
Parental involvement and parenting in diabetes management significantly influence the treatment adherence and metabolic regulation of type 1 DM in preschool-aged children [17]. Type 1 DM in these children requires continuous disease management, especially for children first diagnosed at preschool age; thus, parents play a pivotal role in managing and monitoring diabetes among their children [18,19]. The preschool years present a challenge for self-management, as tasks such as insulin administration, blood glucose monitoring, and control of dietary and physical activity primarily become the responsibility of the parents [10]. Moreover, the child's health, well-being, and disease progression are significantly impacted by the parents' effective management of diabetes. Therefore, when caring for a preschooler with diabetes, it is essential to consider parents the primary targets and provide them with the necessary education and support [10].
Parents of children with diabetes often experience more stress than those with children who do not have diabetes, due to the additional responsibilities of managing the disease. These include administering insulin, controlling diet and blood glucose levels, and limiting physical activity [20]. Parents whose children are diagnosed with type 1 DM at an early age often experience deviations from typical parenting and difficulties adapting due to concerns about managing their child's disease [21]. Approximately 69% of preschoolers experience a temporary recovery in beta-cell function following insulin therapy, resulting in decreases in the required insulin dosage. However, within roughly 12 months, 90% of these children require increased insulin doses [3]. Consequently, parents must adjust to the increased insulin therapy and physiological needs of their child, often finding it difficult to achieve treatment goals [3]. In addition to these challenges, parents also face emotional difficulties due to the prolonged morbidity [3,4]. Recognizing these challenges, the American Diabetes Association considers the perspectives of parents raising children with the disease, as well as those of the children diagnosed with diabetes. The association emphasizes the importance of family-centered care that acknowledges and addresses these difficulties [22].
Contrary to previous suggestions, current nursing interventions focus primarily on children with diabetes, while the parents of these children are not recognized as requiring nursing care [20]. Instead of focusing on preschool-aged children, most studies are conducted on school-age children and adolescents who are capable of partially managing their illnesses [23]. Furthermore, while parents' interest and attention have been directed towards the financial and social challenges of raising a child diagnosed with type 1 DM, their emotional and psychological difficulties have been largely overlooked in the nursing field [22]. When a child is diagnosed with type 1 DM, the whole family may be impacted, as they must reconstruct their daily lives around the child's needs [24]. Consequently, the persistent stress, anxiety, and feelings of helplessness experienced by parents of children with diabetes can hinder their decision-making regarding their children's treatment [22]. The psychological difficulties and burdens faced by parents can influence their children's emotions and disease management, which in turn can impact adherence to treatment [20,25]. Therefore, it is crucial to alleviate the burdens of parents caring for very young children with diabetes, as their well-being is intrinsically linked to their children's psychological, physical, and social development [26].
This integrative review aimed to examine and synthesize prior evidence regarding the burdens of parents with preschoolers diagnosed with type 1 DM. The research questions are "What are the burdens experienced by parents of preschoolers with type 1 DM?" and "Which factors influence these burdens, and what coping strategies can parents employ to mitigate them?"
METHODS
Ethics statement: This study was a literature review of previously published studies and was therefore exempt from Institutional Review Board approval.
1. Study Design
An integrative review was conducted using the framework developed by Whittemore and Knafl [27]. This methodology helps summarize and integrate findings from various methodologies, thereby providing comprehensive evidence on a specific topic [27]. The integrative review process consists of five steps: a) problem identification, b) literature search, c) data evaluation, d) data analysis, and e) presentation. The results of the integrative review were reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [28].
2. Search Methods
This integrative literature review was performed to consolidate the findings of the selected studies. The PRISMA guidelines [28] were employed to facilitate the literature search. Four electronic databases were utilized for this purpose: PubMed, Web of Science, the Cumulative Index to Nursing Allied Health Literature (CINAHL), and PsycINFO. The studies included in this review were published between January 2002 (when the incidence of diabetes in children and preschoolers began to rise) and December 2022. The literature search was conducted by the first author (SC). The search terms used were a combination of the following: type 1 diabetes, DM, insulin-dependent diabetes, parents, caregivers, mother or father, parent, preschoolers, preschool children, early childhood, very young children, burden, stress, fatigue, burnout, and strain. Boolean operators and truncation were employed with combinations of these keywords in an effort to include all relevant articles in the search (Supplement 1).
The inclusion criteria for articles in this study were as follows: (1) original studies published in the English or Korean languages in peer-reviewed journals; (2) in which the study participants were parents of preschool-aged children (3 to 6 years old) [29] who had been diagnosed with diabetes for at least 6 months; (3) for which parents with preschoolers made up more than 50% of the total sample; (4) and relating to the burdens of parents of preschoolers with type 1 DM with various forms of distress such as psychological, emotional, social, or financial (e.g., burden, difficulties, strain, stress, fatigue, or burnout) [30-32]. Systematic literature reviews, opinion pieces, editorials, conference proceedings, and studies published in languages other than English and Korean were excluded from consideration.
3. Search Outcomes
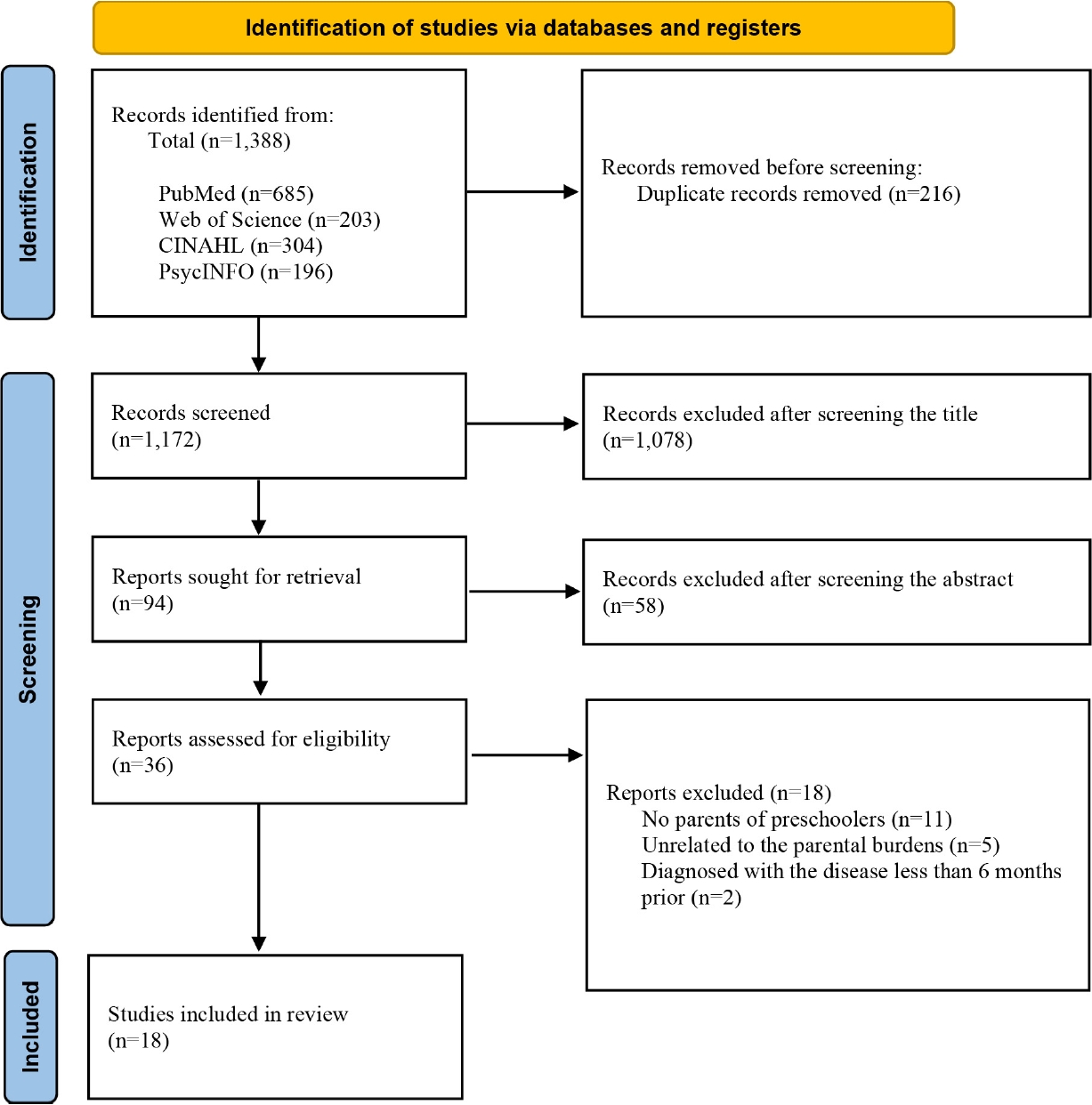
We utilized a PRISMA flowchart [28] for the literature selection (Figure 1). We initially searched a total of 1,388 studies across four databases: PubMed (n=685), Web of Science (n=203), CINAHL (n=304), and PsycINFO (n=196). We then removed 216 duplicate entries and excluded an additional 1,078 articles after screening their titles. After screening the abstracts, we further excluded 58 articles. This left us with 36 articles for full-text review. Of these, 18 articles were excluded for the following reasons: the participants were not parents of preschoolers (n=11), the articles were unrelated to parental burdens (n=5), or the disease had been diagnosed less than 6 months prior (n=2). Ultimately, we selected a final set of 18 articles for inclusion.
4. Quality Appraisal
Two researchers (SC and HS) evaluated the quality of the chosen articles using the Mixed Methods Assessment Tool (MMAT) [33] for each research design. The MMAT is a tool designed to critically appraise the quality of studies with various methodologies, including quantitative, qualitative, and mixed-methods studies [33]. Initially, the researchers independently assessed the chosen studies using two screening questions: a) whether the research questions were clearly defined, and b) whether the data collected were suitable to answer the research questions. Following this, the researchers categorized each article based on its research methodology and evaluated the quality of each article using the MMAT Methodological Quality Criteria. The MMAT tools were used to assess the quality of each study by considering the following criteria: a) the suitability of the research approach and research question, b) the relevance of findings and the collected data, c) the accuracy of the interpretation of results, d) the representativeness of the target population and the suitability of the measurement, and e) the statistical methods used to analyze the results. The researchers responded to each category with either "yes," "no," or "indeterminate" to evaluate the suitability of the chosen studies. The agreement rate was 96.7% (90 item agreements, 3 disagreements). Any discrepancies were discussed by the two researchers until a consensus was reached. No article was excluded after the quality evaluation using MMAT guidelines, as the exclusion of studies could potentially introduce bias [34]. Table 1 presents the quality score of each article.
5. Data Abstraction
Data abstraction was carried out in accordance with the guidelines set by Whittemore and Knafl [27]. We created a tool to condense and scrutinize the data pertinent to the study objective, including the methods, sample, purpose, findings, and strengths and limitations (Table 2). Two researchers independently extracted data from each study using Microsoft Excel (Microsoft Corp.).
6. Synthesis
The researchers meticulously reviewed the chosen studies to extract common content, which they then categorized into individual themes. (Figure 2). The four themes derived from the review were (1) parental burdens, (2) factors related to parental burdens, (3) coping strategies to reduce the burdens, and (4) implications for clinical practice.
RESULTS
1. Characteristics of Selected Studies
Table 2 presents a summary of selected studies published between the years 2002 and 2022. All studies were carried out in Western nations. The studies originated from various countries: one each from Norway [35], the United Kingdom [36], and Hungary [25]; two from the Netherlands [37,38]; and 13 from the United States. The research designs employed in these studies included quantitative studies (14 in total) [23,25,36-47], qualitative studies (3 in total) [35,48,49], and a single randomized controlled trial [50]. The sample sizes in these selected studies varied, ranging from 15 to 597 participants. The participants of these studies were either fathers only (2 studies) [44,46], mothers only (4 studies) [25,36,39,45], or both mothers and fathers (12 studies).
Four studies utilized the State-Trait Anxiety Inventory, developed by Spielberger [51], to measure anxiety symptoms [39,42,45,46]. The Hypoglycemia Fear Survey, created by Cox et al. [52], was used in four studies to gauge parental worry about hypoglycemic symptoms [23,39,41,46]. The stress levels associated with parenting children with DM were measured in four studies [44,46,37,38] using the Pediatric Inventory for Parents, developed by Streisand et al. [53], and in three studies [36,37,44] using the Parenting Stress Index, developed by Abidin [54]. The strengths and limitations of each study are detailed in Table 2.
2. Critique of Selected Studies
Eleven out of 18 studies employed both subjective self-report questionnaires and objective data, including medical records and glycated hemoglobin (HbA1c) levels [23,36-38,40, 42,44,46,48,50]. Objective data in the field of nursing encompass observations, examinations, and results from diagnostic tests [39]. Given the multifaceted nature of health-related concepts, it is advisable to utilize a variety of measurement indicators. These objective data can offer more reliable and valid information compared to subjective data gathered from selfreport questionnaires and interviews [55]. Three studies implemented a qualitative research design [35,48,49]. Qualitative designs delve into the meaning and understanding of phenomena as experienced by individuals in their natural environments [56]. This approach allows for a comprehensive understanding of the experiences, challenges, and burdens faced by parents of preschool children diagnosed with type 1 DM.
However, 17 of the 18 examined studies utilized a cross-sectional design, which complicated the task of tracking changes in parental burdens over time and determining causal relationships between these factors. Only one study employed a longitudinal design [43]. Notably, most participants were well-educated Caucasians earning an average of over $50,000 [23,42,45]. This demographic skew limits the applicability of the findings to parents of lower income brackets or different ethnic backgrounds. A study on atopic dermatitis revealed a similar trend, with lower illness prevalence rates among those in higher socioeconomic positions due to better immune systems [57]. The risk of reporting bias is also present, as most of the selected studies relied on self-reporting methods. Furthermore, none of the studies incorporated a theoretical framework, which should be considered in future research to bolster the validity of the findings. Lastly, all the selected studies were conducted in Western countries. Parenting styles and health-related attitudes can vary greatly depending on race and culture [58]. Conducting more research in Eastern and developing countries could help illuminate these differences and provide valuable insights into how parents manage the health needs of their children diagnosed with type 1 DM.
3. Theme 1: Parental Burdens
Parents bore a variety of burdens, encompassing psychological, physical, and social challenges. They grappled with the psychological burdens of fearing hypoglycemia [23,39,41,46], the stress associated with caring for and managing their children's needs [37,38,42,44,46], depression [39], and anxiety [39, 42,45,46]. Specifically, parents of children with diabetes exhibited higher levels of stress, depression, and anxiety than parents of children without diabetes [25,39,42,47]. In terms of physical symptoms, parents often experienced sleep deprivation due to the need for nocturnal monitoring and blood glucose checks [40,41,45,49]. They expressed feelings of fatigue and being overwhelmed by the responsibilities of child care, which include giving their children undivided attention, preparing meals, and planning activities [38,40,41,48,49]. Parents also perceived burdens in their relationships with others. Parents sometimes focused on caring for their children by reducing social contact and felt uncomfortable disclosing diabetes to acquaintances [35]. Furthermore, parents could be hesitant to interact with other families, recognizing their children's differences due to their illness relative to children without a type 1 DM diagnosis [35].
4. Theme 2: Factors Related to Parental Burdens
The factors contributing to parental burdens were divided into two categories: child characteristics and parental characteristics. Child characteristics associated with increased parental burdens included younger age [41,44], male sex [40], severe diabetes requiring an intensive regimen [23], more behavioral problems [42], poor adherence to treatment [44], a history of hospitalizations or diabetes-related complications [23,40], diabetes-related unconsciousness and seizures [23], and a poor health-related quality of life. In terms of parental characteristics, mothers experienced higher burdens than fathers [38,39]. Factors that exacerbated parental burdens included a low family income [39,44], racial and ethnic minority status [44], rural area of residence [44], a lower level of knowledge about diabetes [36], poor sleep quality [41], low self-efficacy [41,43,46], and low confidence in their ability to manage their child's diabetes [41,46,47].
5. Theme 3: Coping Strategies to Reduce the Burdens
When a child is diagnosed with diabetes, parents often felt overwhelmed and frustrated [48,49]. The burden of trying to resume their normal daily activities while managing their child's condition could be daunting [48]. However, studies found that over time, parents adapted to the situation through support and sharing responsibilities with others, such as a spouse, other family members, and support groups [35,49]. Specifically, mothers coped with the burden by sharing some of the responsibilities of raising and caring for the child with their spouses [49]. Some parents also sought out other caregivers who could provide practical care, such as administering insulin injections [48]. Parents alleviated their burdens by learning more about diabetes and its management [48]. As children grow older, parents found it challenging to strike a balance between control and autonomy [49]. However, they generally recognized that independence and autonomy are essential developmental tasks and thus allow their child to exercise autonomy [49]. In a longitudinal study, half of the parents reported depressive symptoms within 2 months of their child's diabetes diagnosis, but these symptoms decreased by 12 and 18 months post-diagnosis [35]. Additionally, parental self-efficacy in managing diabetes significantly improved from baseline to 12 and 18 months post-diagnosis. Parents rapidly acquired a wealth of information related to diabetes management [59], which enhanced their ability to effectively manage their child's condition [35].
6. Theme 4: Implications for Clinical Practice
Parents expressed a desire to receive direct education from skilled health professionals [35,36,48]. They believed that their burdens could be alleviated through ongoing diabetes education provided by medical staff, and they were particularly interested in learning about the latest technology, potential complications, and overall diabetes management [48]. Parents also sought explanations about possible atypical or non-standard symptoms, especially in early school-age children [36]. They showed interest in contributing to the development of a particular intervention that reflects their preschool-age child's unique characteristics of their preschool-aged children [45]. Furthermore, a child's diabetes diagnosis sometimes required family activities to center around the child, impacting the entire family's life and underscoring the need for the development of family interventions [49]. While maternal stress tended to decrease over time, paternal stress often increased as fathers took on more household responsibilities and care duties [38]. Therefore, it is advisable to develop tailored education programs for parents and provide support for family management. Beyond direct parent training and support, it is also necessary to develop programs that utilize various medical techniques to manage diabetes, which in turn could help alleviate parental stress related to disease management. Recent advances in the treatment of type 1 diabetes, such as the use of continuous subcutaneous insulin infusion and sensor-augmented pumps, are noteworthy in this context [7]. Additionally, child-focused interventions, such as play therapy, have been developed [60]. It is crucial to implement these innovative interventions in preschoolers and assess their effectiveness in this age group to understand their impact on parental burdens.
DISCUSSION
This integrative literature review was conducted to address research inquiries concerning the burden borne by parents of children with type 1 DM diabetes and the factors that influence it. Consequently, four themes were identified: a) parental burdens, b) factors related to parental burdens, c) coping strategies to reduce the burdens, and d) implications for clinical practice. Parents of preschoolers diagnosed with type 1 DM encounter a range of challenges, including psychological burdens such as fear, stress, depression, and anxiety related to managing the disease [46]. The process of accepting the diagnosis and navigating unfamiliar circumstances presents difficulties for parents. They frequently experience clinical levels of anxiety and fears associated with hypoglycemia [39,40], while also expressing concerns about the long-term effects and complications of type 1 DM for their child [40].
Parents experience the physical burdens of caring for children. This is particularly true during the preschool years, when the management of diabetes falls entirely on the parents. Given the physical and cognitive characteristics of this age group, parents often struggle to identify and monitor their children's blood glucose levels [40]. Children under the age of 7 years are susceptible to hypoglycemia due to insulin sensitivity, unpredictable eating habits, and varying exercise behaviors [50]. Moreover, hypoglycemia symptoms in this age group are typically asymptomatic [50], necessitating parents to provide hourly diabetes-specific care to their children [35]. One-third of parents conduct at least one glucose check during the night [50], and those who are more worried about nocturnal hypoglycemia are more likely to perform these checks. This can result in sleep deprivation, leading to daytime dysfunction [41]. A qualitative study found that parents often felt physically pushed to their limits, resulting in constant exhaustion and a decreased sense of restfulness. Consequently, they desired a space where they could rest, separate from their children [35].
Parents often struggle to maintain their relationships with others following their child's diagnosis. Consequently, they tend to withdraw socially as they adjust to their new circumstances shortly after the diagnosis [35]. They then strive to rebuild relationships with their spouses, coworkers, extended family, and other caregivers. Parents must inform medical staff about their child's diabetes and request their understanding and cooperation in managing the condition while the child is under their care [35]. Parents desire the support of secondary caregivers, such as family members, babysitters, and daycare providers, who can share the responsibility of managing the child's diabetes. However, the tasks of identifying, training, and establishing trust with these individuals can also be burdensome [48].
The factors that influence the burdens borne by parents can be categorized into child-related and parent-related characteristics. Child-related characteristics include age, sex, diabetes severity, history of behavioral issues, history of complications, and noncompliance with treatment, all of which can impact parental burdens. Parents of younger children with diabetes tend to more frequently experience higher levels of stress [44], as well as lower self-efficacy [41]. Regression analysis has shown that, when controlling for child age, parents of boys experience higher stress levels than those of girls [40]. Parental anxiety and stress have been significantly linked to behavioral problems in children at mealtime and bedtime [42], as well as to poorer adherence to the child's treatment regimen [44]. Additionally, parental stress levels rise when children have experienced at least one diabetic ketoacidosis event [40]. Parents tend to have more concerns about their children when they are on more intensive medical regimens and have experienced diabetes-related complications, such as unconsciousness or seizures [23].
Parental burdens, such as those related to sex, family income, race, and residential status, are influenced by their socioeconomic characteristics. Furthermore, the degree of parental involvement in diabetes treatment is linked to these burdens. Mothers, who are typically the primary caregivers and are often tasked with managing their children's diabetes, tend to experience higher stress levels than fathers [38]. However, as children grow older, maternal stress levels decrease while paternal levels increase [38]. This shift can be attributed to the changing responsibility of childcare from mother to father, as well as the fact that mothers may become more accustomed to managing diabetes while fathers may have less frequent exposure [38]. Mothers also experience heightened levels of anxiety and depression when their family income is low [39]. Similarly, lower household income has been associated with increased parenting stress [44]. Parents living in rural areas or belonging to racial/ethnic minority groups also tend to have higher stress levels [44]. Parenting stress increases when parents are more involved in treatment [44]. Additionally, parents who are highly involved in managing diabetes often set strict HbA1c goals [61].
A childhood diagnosis of diabetes is life-changing for both the child and family. Parents are often overwhelmed and frustrated upon learning that their child has diabetes. They may feel uncertain about how to adjust to the child's diabetes care [49]. With the diagnosis, parents are assigned roles related to diabetes management alongside their existing roles as parents and can struggle to adapt to their new roles as "guard" [35, page 3]. Parents often feel misunderstood by those outside their immediate circle, aware that their child's condition sets them apart from their peers. This sense of isolation can lead to withdrawal from previously established relationships [35]. Despite these challenges, parents strive to maintain a sense of normalcy in their child's life, often implementing strict dietary rules and restrictions [35]. Parents perceive physical and psychological burdens and attempt to find daycare providers and babysitters who can help them care for the child [48]. However, entrusting others with their child's care and sharing responsibilities can be difficult [48]. By six months to a year after diagnosis, parents have typically gained an understanding of diabetes and learned to adapt to the illness. A higher level of knowledge about diabetes is associated with better treatment adherence and fewer family relationship difficulties [36]. Support groups can provide a valuable outlet for parents, helping to alleviate feelings of loneliness [49]. These parents also learn to share the burden and responsibilities of their child's care with others, such as spouses, family members, and secondary caregivers [35]. As a result, parents often incorporate their child's diabetes care into their routines [35]. This finding aligns with previous research on families of children with chronic illnesses, which found that families often restructure their daily lives to accommodate their child's disease management [62]. Parents tend to worry about their child's safety and may be overly protective. However, as the child matures, parents often aim to transition care responsibilities to that child, supporting them in managing their diabetes independently [49]. This aligns with previous research, which emphasizes the importance of fostering independence in children with chronic illnesses, focusing on their abilities rather than their limitations to promote their development [63,64].
This integrative review revealed that parents often face substantial burdens when a child is diagnosed with diabetes. The stress and burdens borne by parents of children with chronic diseases can impact the children's quality of life [37]. Consequently, it is crucial to comprehend the burdens experienced by parents and devise interventions that can support family functioning and adaptation among children [39]. Specifically, a need exists to offer distinct interventions for parents of very young children (under 6 years) with type 1 DM, which differ considerably from interventions previously provided to parents of children with chronic diseases. Parents of very young children encounter different types of stress and unique experiences [45]. Furthermore, educational intervention is essential, as a greater understanding of diabetes enables parents to implement treatment more effectively and reduces family conflicts [36]. Notably, parents express a desire for direct education from healthcare providers on various topics relevant to diabetes [48]. Educational interventions focusing on diabetes-related knowledge, complications, and childcare skills are required. Parents also seek direct education for secondary caregivers on diabetes management and blood glucose regulation skills, fostering trust and shared responsibility [48].
When a child is diagnosed with diabetes, the dynamics and relationships within the entire family are impacted [65]. Therefore, it is crucial to develop family interventions aimed at alleviating parental stress and burden. A longitudinal study by Nieuwesteeg et al. [37] revealed a correlation between heightened parental emotional involvement, increased discomfort during disease-specific situations, and relatively poor glycemic control in young children with type 1 DM. As such, family interventions are essential to address these issues and enhance glycemic control in this demographic. Furthermore, children with diabetes often exhibit more eating and behavioral problems than their peers, which can exacerbate parental stress and burden. The development of family intervention programs may help alleviate these burdens.
Most papers reviewed for this study utilized a cross-sectional design, which limited our ability to identify changes in parental burdens over time. Further research is needed to understand how these burdens shift according to the child's developmental stage. Additionally, most of the studies focused primarily on mothers, resulting in a dearth of data regarding the paternal perspective. Future research should aim to directly study the burdens experienced by fathers. It is also crucial for future researchers to expand the demographic scope of participants. In this review, most studies predominantly included middle-class, white, and married participants. Family and disease perspectives can vary based on the cultural context, underscoring the need for research conducted in Eastern or Asian countries.
CONCLUSION
This study explored the burdens experienced by parents of preschool-aged children, an area where research and interventions are currently insufficient. During the preschool years, the number of children diagnosed with type 1 DM increases, and the unique developmental characteristics of these children can make parenting and disease management difficult for their parents. The psychological strain and burdens experienced by parents of children with chronic diseases can negatively impact their children's quality of life. Parents of children diagnosed with type 1 DM represent a vulnerable population, and their burdens can influence their children's emotional responses and adaptation to disease management. Therefore, nurses must recognize these parents as targets of nursing care and work to alleviate their emotional difficulties related to child-rearing stress, depression, and anxiety. Future research should focus on developing specific interventions to address these parents' psychological challenges, including tracking parental psychological changes over time. The need should also be considered for nursing interventions for parents of preschoolers, in addition to the nursing education or interventions that have traditionally focused on children of non-preschool ages in clinical settings. By understanding and acknowledging the psychological challenges faced by parents raising preschoolers with type 1 DM, we can help to alleviate the burdens borne by these parents.