AbstractPurposeNursing students are susceptible to medication safety incidents in the neonatal intensive care unit (NICU) related to a lack of communication experience. The purpose of the present study was to investigate the impact of a NICU medication safety simulation (NMSS) focusing on communication clarity, patient hand-off confidence, and patient safety competency in senior-year nursing students.
MethodsThe study utilized a nonequivalent control group pretest-posttest design. In total, 60 nursing students were assigned to two groups. The experimental group participated in the NMSS, which included three medication error scenarios. Pairs of students completed the scenarios together in 10 to 20 minutes. Data were analyzed using the chi-squared test, independent t test, and ANCOVA.
INTRODUCTIONMedication errors in South Korea have steadily increased in the past 4 years, during which 3,798 cases occurred, accounting for 31.8% of patient safety accidents [1]. Medication errors take place in the prescription, distribution, application, monitoring, system, and control processes of administering medication. Since medication errors occur at the individual, system, and management levels in each process, a systematic and complete prevention system should be implemented and errors in individual factors should be identified and educated [2,3]. Errors with the potential to cause harm are eight times more likely to occur in the neonatal intensive care unit (NICU) than in adult settings [1]. Medication errors have a high risk of harming newborns due to their large body surface relative to their low body weight and immature body functions that affect drug absorption, transfer, metabolism, and excretion [4,5]. Despite the utilization of advanced medication injection machines, computerization of prescription systems, and medication safety guidelines to prevent medication errors in the NICU, medication errors in the NICU continue to occur as nurses directly prepare small doses of drugs administered to newborns [1,3,5]. In prescriptions of high-alert medications in the NICU, 64% of medication errors involved the incorrect name or dose of a medication prescribed verbally by doctors communicating to nurses [3]. While teaching students to care for newborns in the NICU is a priority in pediatric nursing curricula, avoiding medication errors has been identified as problematic for learners, as communication problems may contribute to medication errors and nursing students find it difficult to recognize and report such conditions.
Effective communication among medical staff is emerging as the most important competency to prevent medication errors [2]. The US Agency for Healthcare Research and Quality (AHRQ) reported that communication among medical staff is essential for patient safety, and that there is a need for communication competency-based education for patient safety accompanied by thorough monitoring for medication safety management [6]. According to priming patient safety theory, safety nursing hand-off communication elicited a change in nursing safety-oriented behavior [5]. Nurses subsequently prioritize and are motivated to perform tasks and risk assessments related to achieving patient safety. These efforts continue until nurses mitigate identified risks and errors during the patient care encounter. Hand-off communication involves more than information transfer, and the consequences of hand-off communication for multi-functional, situated routines extend beyond patient safety [5]. SBAR (situation, background, assessment, recommendation) is a standardized method for efficient communication among medical staff aiming to deliver fast and correct information about patients' conditions in emergencies, and it has been shown to reduce harmful accidents [7]. Although studies on patient safety competency have confirmed that SBAR training improves communication skills, relatively few studies have applied SBAR to strengthen nurses' hand-off communication ability during the routine practice of medication [8,9].
The use of simulations is supported by the Institute of Medicine as a strategy to improve patient safety and support the transfer of learning to the clinical setting [2]. Simulations provide an opportunity to demonstrate clinical judgment and make decisions in a safe environment while witnessing the consequences and evaluating the effectiveness of actions [6,7]. Simulation-based emergency airway management education for NICU nurses improved their problem-solving ability and clinical performance confidence [10]. Bonds [7] utilized SBAR in a simulation, resulting in nurses gaining practice with communicating more effectively to their individual disciplines with the patient safety competency. Although simulations have been suggested as a highly useful strategy to increase communication skills and safety competency [4,5], insufficient studies have investigated simulations dealing with NICU medication safety for nursing students.
An integrated review study concluded that communication clarity and patient hand-off confidence prevent serious medication errors and increase patient safety competency, and simulations included using SBAR to report medication errors to nurses and medical staff, as well as knowing safe medication administration practices in the NICU [6-9]. Therefore, this study aimed to develop a NICU medication safety simulation (NMSS) focusing on communication and to evaluate its effects on nursing students' communication clarity, patient hand-off confidence, and patient safety competency.
METHODS
Ethics statement: This study was approved by the Institutional Review Board (IRB) of Konkuk University (No. 7001355-202002-HF-365). Informed consent was obtained from all participants.
1. Study DesignThe NMSS in this study integrated the Healthcare Simulation Standards of Best Practice (HSSBP), which include communication clarity using high-fidelity mannequins, as well as knowledge of the significance and application of safe medication administration practices. This study used a quasiexperimental pretest and posttest design and followed the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) guidelines [11].
2. ParticipantsAfter institutional review board approval was obtained, a convenience sample of senior-year nursing students at a University in Chungju, South Korea enrolled in this study. The number of participants was calculated using G*Power 3.1.9.4 [12]. Based on previous studies that utilized the independent t test in interventions involving nursing students, with an effect size of 0.35, a significance level of 0.05, power of 0.80, two groups, and two measurement points, the required number of participants per group was at least 26 [9,10]. Thirty participants in each group were recruited considering a potential dropout rate of 20%. However, no participants dropped out, and 60 participants were included in the final data.
3. The Neonatal Intensive Care Unit Medication Safety SimulationThe NLN Jeffries Simulation Theory [13] and HSSBP [2] provided theoretical support for this study (Table 1). The NLN Jeffries Simulation Theory identifies components of simulation design and implementation, including the stages of analysis, design, development, implementation, and evaluation [13]. The HSSBP was developed to support quality in simulation design and implementation [2,7].
In the analysis stage, the learning needs of senior students who had taken pediatric nursing coursework and had practical experience were investigated, and efficient communication methods for medication safety were reviewed by analyzing the HSSBP and materials from the AHRQ. Previous studies were also reviewed in order to derive core competencies for NICU communication.
In the design stage, the learning goals of medication safety were reviewed and classified into three domains (knowledge, skills, and attitudes), the learning outcomes of the Korean Accreditation Board of Nursing Education were applied, and the learning content was chosen (monitoring and reporting medication errors for premature infants in the NICU). Learning took place through high-fidelity simulation practice based on the Jeffries model. The NMSS fostered curiosity and learning motivation among learners through their orientation in the participation process, explored nursing problems in group discussions of medication error scenarios in premature infant care, and encouraged learners to explain and apply key concepts related to communication with staff through simulations. The evaluation stage included self-evaluation and a reflection diary. As learning media, video lectures, computer programs, high-fidelity simulators, audio/video systems, practical equipment, and handouts were used.
In the development stage, the data and content from the analysis and design stages were converted into a program. The content validity was verified by experts (simulation specialists and two nurses who had more than 10 years of NICU work experience) to confirm the suitability of the developed learning materials. After piloting the program with two students who were not included among the study subjects, the final module of the NMSS was developed through correction and supplementation.
The module was designed in three stages (pre-briefing, scenario-based performance, and debriefing), and it lasted for a total of 130 to 140 minutes (Table 1).
Participants studied the learning guide related to medication safety in advance and watched videos to enhance their understanding of the SBAR method as preparatory work. The learning guide consisted of communication clarity and medication safety in the NICU, dealing with causes of medication errors, clinical symptoms, nursing assessment, reporting and patient hand-off, clinical case studies, SBAR communication forms, and related video links. The reliability and validity testing regarding the learning guide design, simulation scenario development, and assessment tools was conducted by two child health nursing professors and one nurse who had more than 10 years of NICU work experience. During the subsequent orientation session, the instructor reviewed what students had studied, the simulation situation was introduced, and clinical case-based training was conducted. The instructor in this study was highly educated, with a specialization in child health nursing, and had more than 5 years of experience providing lectures and 3 years of simulation education. The clinical cases dealt with the importance of monitoring for medication safety, medication errors due to inaccurate verbal prescriptions, and adverse events due to a lack of communication between medical staff. Students acted as nurses through role play and used the SBAR format to report patient hand-offs and medication errors that occurred in each case.
The NMSS scenario involved a premature infant with dyspnea. The scenario topics included frequently occurring situations in the NICU, such as monitoring the patient's status in case of medication errors related to the dosage calculation, intravenous administration, high-alert medication procedures, hand hygiene, checking laboratory values and vital signs before administering medication, checking electronic medical record (EMR) prescription errors, and reporting medication errors to medical staff. Each scenario integrated information collection and analysis regarding the medication error situation to foster learners' ability to make judgments on the clinical situation, report the situation afterward, and make suggestions for problem-solving. For example, the student performs a physical assessment due to the subject's fast respiratory rate, discovers that the total parental nutrition injection rate is too fast, rechecks the prescription, and reports a medication error quickly to doctors and hands the case off to a nurse.
In the process of implementation, pairs of students completed the scenarios together using high-fidelity mannequins in the laboratory equipped with a simulation room with a one-way mirror, which was done to evaluate the communication process of monitoring medication errors and reporting to medical staff by phone. Four teams per group consisted of 7 to 8 students. Each pair took 10 to 20 minutes to perform the scenario. After the scenario was over, students filled out a reflection diary. At the end of the NMSS, students were debriefed in groups using SBAR, with an emphasis on effective communication for safe medication. The instructor led the debriefing as appropriate to assist in aligning students' efforts with the scenario objectives. The instructor and study team members were trained in conducting the NMSS and debriefing by the principal investigator (PI).
This study was arranged in the following order: pretest, intervention (NMSS), and posttest (Figure 1). Prior to the intervention, the experimental and control groups were surveyed on their general characteristics, communication clarity, patient hand-off confidence, and patient safety confidence. Potential covariates such as age, gender, professional satisfaction, and clinical practice satisfaction were included as general characteristics. The experimental group received the learning guide and participated in the NMSS once, while the control group only received the learning guide. The learning guide consisted of three topics: safety nursing practice, effective communication, and SBAR reporting related to medication errors in the NICU. The participants' performance in the experimental group was verified through video recordings in order to increase the evaluation accuracy and decrease bias between instructors. The inter-observer reliability between the instructors was above 0.90 in this study. The post-test was completed after the intervention using the same questionnaire as in the preliminary survey. After all the investigations were completed, the instructor provided the NMSS to interested students in the control group.
4. Research Tools1) Communication clarityThis study used a patient safety communication competency tool that Cho [14] translated, modified, and supplemented based on the tool that Marshall et al. [15] developed to evaluate the content and clarity of reports for medical students; approval was obtained for the use of the tool. The tool consists of 14 questions, and the response to each question is on a 5-point Likert scale ranging from "strongly disagree" (1 point) to "strongly agree" (5 points). A higher score indicates higher communication clarity. In Cho's study [14], Cronbach's ⍺ was .77, and in this study, it was .91.
2) Patient hand-off confidenceLewis et al. [16] developed a tool for rehabilitation treatment students, which was adapted by Kwong [17] to reflect hand-off situations and other contexts in which nursing students communicate with nurses; approval was obtained for the use of the tool. This tool consists of 14 items in three areas: anxiety, confidence, and SBAR use. Each question is on a 5-point Likert scale ranging from "strongly disagree" (1 point) to "strongly agree" (5 points). A higher score indicates higher patient hand-off confidence. In Kwong's study [17], Cronbach's ⍺ was .80, and in this study, it was .79.
3) Patient safety competencyTo measure patient safety competency, including safe medication administration, this study used the patient safety competency tool developed by Lee et al. [18], and approval was obtained from the tool developer. This tool is a self-report questionnaire, divided into three domains: knowledge, skills, and attitudes. There was a total of 41 questions: six questions for knowledge, 21 questions for skills, and 14 questions for attitudes. The responses are measured on a 5-point Likert scale; a higher score indicates higher patient safety competency. In the study of Lee et al. [18], Cronbach's ⍺ was .90, and it was .94 in this study.
5. Data CollectionBefore conducting this study, approval was granted by the IRB, with which one of the researchers is affiliated. Participants enrolled voluntarily and were informed of their right to decline participation without disadvantage. Participants' simulation scores were not included in their grades. The purpose, content, period, methods, and ethical considerations, such as the fact that the collected data would be used only for research purposes, were explained to the participants by PI. The PI and study team members remained blinded to the group assignment until the conclusion of the study session. After being consented by the PI, participants were divided into class A and class B using the existing class arrangement. Among students in class A, those who wanted to participate in the program were assigned to the experimental group. Class B was assigned to the control group in the same way.
Data collection began with the control group to minimize the possibility of information sharing, which could have affected the outcomes, from May 2020 to July 2020. The experimental group filled out a pretest questionnaire before the NMSS. After the end of the 2-week program, the posttest was conducted using the same questionnaire. Each questionnaire took approximately 20 minutes to complete. The control group received the pretest and was provided a learning guide for NICU communication, and the posttest was conducted 2 weeks later. Both the experimental group and the control group received small gifts for participation.
6. Data AnalysisThe data were analyzed using IBM SPSS for Windows version 23.0 (IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test was performed to test the normality of the distribution of data on participants' variables, and the general characteristics were analyzed using means, standard deviations, real numbers, and percentages. The chi-squared test and the independent t test were used to test the two groups' general characteristics and the prior homogeneity of the variables. To understand the effects of the intervention, the independent t test was used [9]. Patient hand-off confidence showed a significant difference in the pretest, and was analyzed using ANCOVA using the pretest values as a covariate.
RESULTSThe general characteristics did not show significant differences between the experimental group and the control group. For the pretest variables, there were no significant differences in communication clarity and patient safety competency between the two groups (Table 2). According to the Kolmogorov-Smirnov analysis results, all variables had a normal distribution (p>.05).
The mean differences in scores for communication clarity, hand-off confidence, and patient safety competency between the groups are presented in Table 3. The pre-post test scores for the variables were analyzed using the independent t test. The experimental group had significantly higher scores for communication clarity and patient safety competency than the control group (Figure 2). Communication clarity demonstrated a significant increase, with scores of 4.14±0.09 in the experimental group and 4.00±0.08 in the control group at the posttest (t=2.23, p=.015) (Figure 2). For patient safety competency, a statistically significant difference was found, with scores of 4.13±0.80 in the experimental group and 3.78±0.08 in the control groups (t=4.06, p<.001) (Figure 2). However, the score for the subdomain of attitudes did not show a significant difference in this regard (Table 3).
For the patient hand-off, between-group scores were compared using ANCOVA. Using the pretest values as covariates, patient hand-off confidence scores significantly increased in the posttest, with 3.16±0.08 points in the experimental group and 3.03±0.08 points in the control group (F=5.18, p=.027) (Table 3, Figure 2).
DISCUSSIONThis study was conducted to develop and verify the effectiveness of simulation education for enhancing communication clarity, patient hand-off confidence, and safety competency in situations related to medication errors in the NICU for nursing students.
First, the NMSS improved nursing students' communication clarity. This is similar to the result found in a study [18] that provided team-based simulation practice applying SBAR for nursing students, resulting in improved communication clarity. Another study also found that nursing students' communication skills and self-efficacy in communication were improved by a program in which students practiced frequent communication situations in clinical settings [19]. SBAR, a structured communication tool that includes the patients' current problems, medical history, current symptoms, and vital signs and nurses' recommendations, facilitated effective communication between nurses and physicians in the NICU. Because ineffective communication among health care team members contributes to patient harm and adverse medication errors, communication clarity becomes instrumental in preventing negative patient outcomes. Role play based on a real case scenario in simulations provides learners with targeted communication practice and feedback to acquire and thereby improve communication clarity with each other in various situations. Hence, we believe that the NMSS could allow students to train themselves on how to handle NICU medication errors according to real nurses' roles through scenario-based learning, as well as an opportunity to learn SBAR reporting. Continued education and training on communication for nursing students will help them strengthen their patient safety competency and improve the quality of nursing care when they become new nurses.
Second, this simulation improved nursing students' hand-off confidence. This is similar to the finding of a previous study that nursing students who participated in hand-off simulation practice had higher hand-off confidence than those who only participated in the general practice [20]. However, this result was different from Park and Im's study [21], in which a hand-off simulation practice was conducted and it was found that the hand-off confidence improved, but the hand-off performance capability did not. The above considerations suggest that effective debriefing is important in simulation practice. In this study, two factors appear to have contributed to improving hand-off confidence: 1) repeatedly providing training on hand-off methods using SBAR in the event of a medication error through lectures, videos, clinical case studies, and simulation practice; and 2) documenting the hand-off process in person immediately after scenario performance and conducting a debriefing to check their shortcomings by observing recorded videos. In the debriefing process, students had time to reflect on and reorganize their simulation practice experience. Since patient hand-offs among nurses are an important communication process for improving nursing quality and patient safety, there is a need for structured and standardized communication techniques such as SBAR along with the implementation of checklists to reduce safety errors [22]. To enhance nursing students' hand-off confidence, repeatedly educating them through simulations of specific situations is necessary.
Third, the implementation of NMSS was effective in increasing patient safety competency. This is similar to Park's study [23], in which a risk prediction simulation for nursing students improved self-efficacy regarding patient safety. This is also similar to a study finding that team-based simulation exercises on patient safety for nursing students and interns in internal medicine led to improved confidence in patient safety [24]. Nurses' high workload in the NICU due to the use of high-alert medications and the considerable variety of medical equipment, given the characteristics of newborns, could increase their vulnerability to patient safety incidents such as medication errors [21]. The NMSS improved nursing students' understanding of medication errors based on priming patient safety theory. It also provided opportunities to self-determine the causes and solutions for medication errors that frequently occur during routine work in the NICU, considering the use of TPN, fat emulsion, fentanyl, and anti-infective agents, as well as EMR prescription errors. In addition, SBAR communication is a technique designed to facilitate effective and direct communication among medical staff in busy situations, and it features a short, structured, and predictable format for the effective delivery of important information in the NICU.
In this study, significant differences between the two groups were found in patient safety knowledge and skills, but not in attitudes. These findings indicate that the NMSS may be an effective method for educating nurses about patient safety knowledge and skills. These findings are consistent with the existing literature identifying that simulations can enhance safety education programs in the NICU [25]. Although patient safety attitudes did not show a statistically significant difference between groups, the pre-posttest difference in attitudes showed a slightly greater decrease in the experimental group than in the control group. Attitudes toward patient safety included recognition of the organizational culture related to patient safety, the use of standardized systems such as information technology and electronic data processing systems for patient safety, and negative perceptions of errors; thus, it might not be reasonable to expect that a single educational session would improve students' attitudes [7,21,23]. According to the students' reports, students' negative perceptions and attitudes toward medication errors became stronger, and communication in a structured process became stressful and more burdensome after exposure.
In addition, NICU nurses may not consider that they contribute to patient safety through their constant routine actions to manage risk [6,25]. For example, the goal of working with a clean syringe pump motivated actions such as checking the machine's operation; however, those actions also decreased the risk of infection, supporting the goal of patient safety. The way to improve students' patient safety attitudes is to avoid creating a task mindset, and instead foster an outcome focus that emphasizes the connections between nursing interventions and patient safety attitudes. The NMSS training program, with its focus on medication tasks using high-fidelity simulation scenarios, followed by debriefing, may be an evidence-based approach for helping nursing students improve their patient safety attitudes.
This study is meaningful in that it developed a simulation program consisting of theoretical education, case-based practice training, and simulation practice realistically reflecting medication errors in the NICU. Scenarios should incorporate key messages into patient safety processes rather than simply creating a single medication error to address an individual communication ability. The simulation had beneficial effects not only on medication safety confidence and competence, but also on SBAR reporting and medication safety actions in the process of routine tasks. It is also significant that the simulation improved the safety competencies of nursing students, including communication clarity and hand-off confidence, which are applicable to the clinical field.
The results of this study have limited generalizability because they were obtained from students at a single institution instead of using a randomized controlled design. Although we attempted to minimize confounding factors separately through group assignment, convenience-based allocation may not have been excluded completely. Another limitation is the failure to account for potential confounding variables, including the type of clinical experiences, academic performance, and school satisfaction. This program explored only the short- term impact on nursing students' patient safety competency. Therefore, we propose a study to identify the long-term effects of the patient safety program on nursing students' patient safety-related competency when they work in clinical settings as new nurses. In addition, we suggest conducting further research to verify the effects of this program by developing scenarios for NICU patient safety incidents other than medication errors.
CONCLUSIONNewborns admitted to the NICU are vulnerable to medication error incidents, underscoring the need for communication clarity practice for nursing students in the NICU. Nursing students already have the goal of patient safety as a result of their pediatric nursing education and training; however, unexpected routine demands in the NICU for nursing time and attention can cause medication errors. The pediatric nursing curriculum should include medication safety theory and skills beyond the "Five Rights" construct. Furthermore, nursing educators must guard against viewing the goal of patient safety as a singular or one-time intervention.
This study implemented a simulation program using SBAR that incorporated communication clarity and patient hand-off confidence and patient safety competency. The findings provide evidence supporting the effect of communication simulations on expanding nursing students' understanding of medication safety in the NICU. Communication simulation will help provide education that involves various scenarios and repeated feedback, so that nursing students will be adequately trained in medication safety. Effective communication with SBAR documentation could serve as a surrogate marker during critical patient events in the NICU.
NotesAuthors' contribution
Conceptualization: Eun Sun Ji; Data collection: Minyoung Yim; Formal analysis: Mi Seon Son; Writing-original draft: all authors; Writing-review and editing: Eun Sun Ji; Final approval of the published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
REFERENCES1. Korea Institute for Healthcare Accreditation. Korean patient safety incident report 2020 [Internet]. Sejong Ministry of Interior And Safety; 2020 [cited 2021 October 19]. Available from: https://www.urology.or.kr/rang_board/list.html?num=15656&start=45&code=notice
2. National Academies of SciencesSciences, Engineering, and Medicine.. Assessing progress on the institute of medicine report: the future of nursing. Washington, D.C: The National Academies Press; 2016. p. 1-220. https://doi.org/10.17226/21838
3. INACSL Standards Committee. Healthcare Simulation Standards of Best PracticeTM professional development. Clinical Simulation in Nursing. 2021;58:5-8. https://doi.org/10.1016/j.ecns.2021.08.007
4. D'Errico S, Zanon M, Radaelli D, Padovano M, Santurro A, Scopetti M, et al. Medication errors in pediatrics: proposals to improve the quality and safety of care through clinical risk management. Frontiers in Medicine. 2022;8:814100. https://doi.org/10.3389/fmed.2021.814100
5. Groves PS, Bunch JL. Priming patient safety: a middle-range theory of safety goal priming via safety culture communication. Nursing Inquiry. 2018;25(4):e12246. https://doi.org/10.1111/nin.12246
6. Schmidt J, Gambashidze N, Manser T, Guß T, Klatthaar M, Neugebauer F, et al. Does interprofessional team-training affect nurses' and physicians' perceptions of safety culture and communication practices? Results of a pre-post survey study. BMC Health Services Research. 2021;21:341. https://doi.org/10.1186/s12913-021-06137-5
7. Bonds RL. SBAR tool implementation to advance communication, teamwork, and the perception of patient safety culture. Creative Nursing. 2018;24(2):116-123. https://doi.org/10.1891/1078-4535.24.2.116
8. Muller M, Jurgens J, Redaelli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018;8(8):e022202. https://doi.org/10.1136/bmjopen-2018-022202
9. Uhm JY, Ko Y, Kim S. Implementation of an SBAR communication program based on experiential learning theory in a pediatric nursing practicum: a quasi-experimental study. Nurse Education Today. 2019;80:78-84. https://doi.org/10.1016/j.nedt.2019.05.034
10. Ji EA. Development and evaluation of extremely low birth weight infant nursing simulation education program for nurses in neonatal intensive care unit. Journal of Korea Academia-Industrial cooperation Society. 2022;23(5):321-333. https://doi.org/10.5762/KAIS.2022.23.5.321
11. Des Jarlais DC, Lyles C, Crepaz N, TREND Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. American Journal of Public Health. 2004;94(3):361-366. https://doi.org/10.2105/ajph.94.3.361
12. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behavior Research Methods. 2009;41(4):1149-1160. https://doi.org/10.3758/BRM.41.4.1149
13. Jeffries PR. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nursing Education Perspectives. 2005;26(2):96-103.
14. Cho HJ. The effect of SBAR program education on a nurse's communication clarify and self expression [master's thesis]. Seoul: Yonsei University; 2013. p. 1-58.
15. Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Quality & Safety in Health Care. 2009;18(2):137-140. https://doi.org/10.1136/qshc.2007.025247
16. Lewis M, Bell J, Asghar A. Use of simulated patients in development of physiotherapy students' interpersonal skills. International Journal of Therapy and Rehabilitation. 2008;15(5):221-229. https://doi.org/10.12968/ijtr.2008.15.5.29234
17. Kwong AYY. Using a standardized communication tool SBAR to improve LVN students' shift reporting [dissertation]. San Francisco (CA): University of San Francisco; 2011. p. 1-149.
18. Lee NJ, An JY, Song TM, Jang H, Park SY. Psychometric evaluation of a patient safety competency self-evaluation tool for nursing students. Journal of Nursing Education. 2014;53(10):550-562. https://doi.org/10.3928/01484834-20140922-01
19. Kim SJ, Kim B. Effects of communication empowerment program based on situated learning theory for nursing students. Journal of Korean Academy of Nursing. 2018;48(6):708-719. https://doi.org/10.4040/jkan.2018.48.6.708
20. Kim SK, Seo MS. Effect of hand-over simulation education in the hand-over self efficacy, performance competency, and communication capacity using PASS-BAR for nursing university students. Journal of Learner-Centered Curriculum and Instruction. 2020;20(15):309-330. https://doi.org/10.22251/jlcci.2020.20.15.309
21. Park SN, Im YS. Utilizing video vs simulation practice for handoff education of nursing students in pediatric nursing. Child Health Nursing Research. 2018;24(1):27-36. https://doi.org/10.4094/chnr.2018.24.1.27
22. Rhudy LM, Johnson MR, Krecke CA, Keigley DS, Kraft SJ, Maxson PM, et al. Standardized change-of-shift handoff: nurses' perspectives and implications for evidence-based practice. Association of Critical-Care Nurses. 2022;31(3):181-188. https://doi.org/10.4037/ajcc2022629
23. Park JH. The effects of simulation program by applying hazard perception training on self-efficacy of patient safety, error recovery and problem-solving process in nursing students. Journal of Korea Society for Simulation in Nursing. 2016;4(1):23-32.
24. Goolsarran N, Hamo CE, Lane S, Frawley S, Lu WH. Effectiveness of an interprofessional patient safety team-based learning simulation experience on healthcare professional trainees. BMC Medical Education. 2018;18(1):192. https://doi.org/10.1186/s12909-018-1301-4
25. Chatziioannidis I, Mitsiakos G, Vouzas F. Focusing on patient safety in the neonatal intensive care unit environment. Journal of Pediatric and Neonatal Individualized Medicine. 2017;6(1):e060132. https://doi.org/10.7363/060132
Figure 1.Process of data collection for the neonatal intensive care unit medication safety simulation for nursing students. CC, communication clarity; Cont., control group; Exp., experimental group; NMSS, neonatal intensive care unit medication safety simulation; PHC, patient hand-off confidence; PSC, patient safety competency. 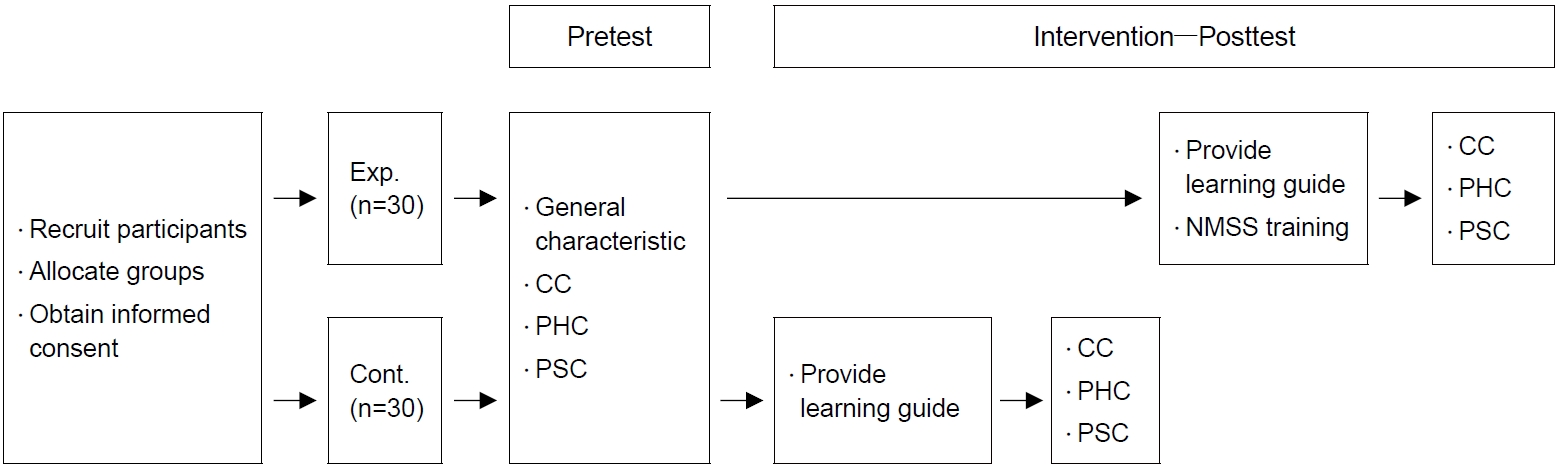
Figure 2.Pretest-posttest mean differences in communication clarity, patient hand-off confidence, and patient safety competency between the groups. (A) Communication clarity. (B) Patient hand-off confidence. (C) Patient safety competency. Cont., control group; Exp., experimental group; Post, posttest; Pre, pretest. 
Table 1.Procedure of the Neonatal Intensive Care Unit Medication Safety Simulation BP, blood pressure; CA, corrected age; EMR, electronic medical record; GA, gestational age; HR, heart rate; ID, identification; IV, intravenous; NICU, neonatal intensive care unit; RR, respiratory rate; SBAR, situation, background, assessment, recommendation; SMOF, soya oil triglycerides, medium chain, olive oil, and fish oil; SpO2, saturated oxygen; TPN, total parenteral nutrition; UVC, umbilical vein catheter. Table 2.Homogeneity of the General Characteristics and Outcome Variables of Groups (Communication Clarity, Patient Hand-off Confidence, and Patient Safety Competency) (N=60) Table 3.Pretest-Posttest Mean Differences of Communication Clarity, Patient Hand-off Confidence, and Patient Safety Competency between the Experimental and Control Groups (N=60)
|
|