Participation in and perceptions of antibiotic stewardship behaviors among nurses at a children’s hospital in South Korea: a descriptive study
Article information
Abstract
Purpose
This study investigated participation in and perceptions of antibiotic stewardship among nurses at a children's hospital.
Methods
This descriptive study included 125 nurses working in the inpatient ward, intensive care unit and emergency room of a single tertiary children's hospital. The study measured 14 factors influencing antibiotic stewardship behaviors using the theoretical domains framework. Each factor was analyzed by categorizing it into components (capability, opportunity, and motivation) that have been proposed as influencing factors in the COM-B model of behavior. One-way analysis of variance and Pearson correlation coefficients were used to explore differences in antibiotic stewardship behaviors and influencing factors according to general characteristics and the correlation between antibiotic stewardship behaviors and COM-B components.
Results
No statistically significant difference in antibiotic stewardship behaviors was found based on the experience of antibiotic stewardship education or the nursing department. However, significant differences were observed in the perception levels of factors related to antibiotic stewardship behaviors according to the experience of antibiotic stewardship education in skill (physical) (p=.042), knowledge (p=.027), intentions (p=.028), and social influences (p=.010). Additionally, significant differences were observed in perception levels according to the sub-components of the COM-B model, specifically physical capability (p=.042), psychological capability (p=.027), and social opportunity (p=.010).
Conclusion
To expand nurses' involvement and roles in antibiotic stewardship, nurses should acknowledge the significance of appropriate antibiotic use, aiming to enhance the quality of medical care and ensure patient safety. In pursuit of this objective, tailored education aligning with the specific needs and practices of nurses is essential.
INTRODUCTION
It is undeniable that the development and widespread use of antibiotics have revolutionized the management of infectious diseases. However, the emergence of antibiotic resistance has become a global concern. With limited progress in the development of new antibiotics, the spread of antibiotic resistance poses a significant threat to public health. The consequences of antibiotic resistance include worsening patient outcomes and increasing medical costs [1]. According to a report by Jim O'Neill, approximately 700,000 people worldwide die each year from infections caused by antibiotic-resistant bacteria. If the issue of antibiotic resistance is not addressed, projections suggest that by 2050, there could be as many as 10 million deaths annually due to antibiotic-resistant infections, with economic losses potentially reaching 100 trillion dollars [2].
In response to this critical situation, the World Health Organization declared antibiotic resistance a major health crisis that endangers human life and introduced a global action plan in 2015 [3]. Similarly, the Korean government tackled this issue by unveiling the National Antibiotic Resistance Management Plan (2021–2025) at the ministry level in 2021. This national plan prioritizes the appropriate use of antibiotics, with a key task being the introduction and promotion of antibiotic stewardship programs in medical institutions [4].
The increasing use of antibiotics, along with their misuse, is contributing to the growth of antibiotic resistance. This escalation in resistance results in greater dependence on broad-spectrum antibiotics, which in turn leads to more misuse, creating a harmful cycle. Breaking this cycle is critical, and to do so, proactive management of antibiotic use must be implemented. These programs are designed to encourage the responsible use of antibiotics, which can improve patient outcomes and reduce the negative consequences of antibiotic use. These consequences include higher medical expenses, the development of antibiotic-resistant bacteria, and conditions such as Clostridioides difficile-induced enteritis [5].
Antibiotic stewardship involves coordinated interventions designed to improve and evaluate the appropriate use of antibiotic agents. It promotes the selection of the optimal antibiotic regimen, taking into account factors such as dosing, duration of therapy, and route of administration. The primary goal of antibiotic stewardship is to achieve the best clinical outcomes related to antibiotic use while simultaneously minimizing toxicity and other adverse effects. In doing so, antibiotic stewardship seeks to limit the selective pressure exerted on bacterial populations, thus reducing the development of antibiotic-resistant strains [1].
In essence, antibiotic stewardship can be defined as a comprehensive strategy that aims to prevent the spread of antibiotic resistance, enhance patient safety, and improve the quality of medical care by ensuring antibiotics are used wisely. The term “antibiotic stewardship” appears across various contexts in the literature and embodies several core concepts: (1) controlling antibiotic use, which involves the careful management of antibiotics to select the most suitable treatment, taking into account the correct dose, duration, and route of administration; (2) optimizing clinical outcomes, which focuses on achieving the best possible clinical results while minimizing adverse effects and the risk of developing antibiotic resistance; (3) integrated interventions, which refer to a suite of coordinated measures designed to evaluate, improve, and promote the proper use of antibiotics. A multifaceted approach involves a variety of strategies, including policies, guidelines, surveillance, education, and audits. These are five key components identified as crucial elements in preventing the emergence of antibiotic resistance. Responsible use of antibiotics focuses on maximizing their effectiveness both in the present and for future generations. This entails judicious use that prevents unnecessary usage and ensures targeted, limited treatment [5].
The pathogens responsible for healthcare-associated infections and their antibiotic resistance patterns differ significantly between adult and pediatric patients [6,7]. Moreover, the infectious diseases commonly seen in children, along with their symptoms and trends in antibiotic susceptibility, are distinct from those observed in adults. Additionally, the pharmacokinetic and pharmacodynamic properties of drugs in pediatric patients are influenced by factors such as age, weight, and the presence of disease. These differences underscore the importance of creating antibiotic stewardship guidelines that are specifically designed for the pediatric population [8]. In recognition of the unique needs of pediatric patients, the “Guidelines for Developing an Institutional Program to Enhance Antibiotic Stewardship” issued by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America highlight the necessity of assessing the effectiveness of antibiotic stewardship in hospitalized patient subpopulations, including neonates, infants, and children. This assessment is identified as a top research priority, underlining the critical need for antibiotic stewardship strategies that are tailored to pediatric populations [9].
The successful implementation of antibiotic stewardship requires collaboration among a diverse group of healthcare professionals, such as doctors, pharmacists, nurses, microbiologists, infection prevention specialists, and information technology experts. Nurses, in particular, with their pivotal role in patient care workflow and communication, are essential to the success of antibiotic stewardship programs [10]. In developed countries, there is an increasing recognition of the substantial role that nurses play in antibiotic stewardship, and their involvement is being acknowledged more frequently [11].
In the United States, the critical role of nurses in antibiotic stewardship has been emphasized by the Centers for Disease Control and Prevention (CDC). The Core Elements of Hospital Antibiotic Stewardship Programs: 2019 includes nursing-based interventions, underscoring the indispensable contributions of nurses to these initiatives [11]. Nurses are instrumental in ensuring the appropriate use of antibiotics through a range of key responsibilities. These include collecting specimens correctly before starting antibiotic therapy, interpreting microbiological test results to assist physicians in choosing the best antibiotics or deciding when to stop them, monitoring for early signs of bacterial infection to initiate antibiotics promptly, engaging in the assessment and discussion of antibiotic usage and de-escalation strategies, providing guidance on intravenous and oral antibiotic administration, verifying antibiotic allergies in patient histories, and educating patients and their families about antibiotic treatments [12,13].
While numerous international guidelines stress the critical role of nurses in the success of antibiotic stewardship programs, there is a notable lack of knowledge and awareness among Korean nurses about antibiotic stewardship in certain regions. Additionally, the precise role of nurses within these programs has yet to be clearly delineated, highlighting the need for additional research in this area [14].
In addition, a growing body of evidence supports the efficacy of antibiotic stewardship programs in reducing antibiotic overuse and enhancing patient outcomes across various pediatric settings [15]. However, implementing recommendations in acute pediatric settings presents unique challenges due to the vulnerability and complexity of the patient population. Pediatric nurses play a pivotal role in collaborating with both parents and children to ensure that consumers are well-informed and actively involved in these critical aspects of their care [16]. Despite this, research on antibiotic stewardship participation and the factors influencing it among nurses working in children's hospitals has been limited.
In this study, we utilized the theoretical domains framework (TDF) to understand the determinants of behavior. The TDF was created through a collaborative effort between behavioral scientists and implementation researchers. They identified key theories related to implementation and organized the constructs from these theories into domains [17]. This effort resulted in the integration of 33 behavior and behavior change theories into 14 domains: “knowledge,” “skills,” “social/professional role and identity,” “beliefs about capabilities,” “optimism,” “beliefs about consequences,” “reinforcement,” “intentions,” “goals,” “memory, attention and decision processes,” “environmental context and resources,” “social influences,” “emotions,” and “behavioral regulation” [18]. The TDF provides a comprehensive set of potential mediators for behavior change, particularly in relation to clinical actions [19]. It is an invaluable conceptual tool for investigating implementation challenges, designing interventions to improve healthcare practices, and comprehending the processes of behavior change in the implementation of evidence-based care [19].
In intervention design, the TDF effectively aligns with the behavior change wheel (BCW) [18]. The BCW defines the target behavior using the capability, opportunity, and motivation model (the COM-B system), where capability encompasses both psychological and physical components, opportunity includes social and physical elements, and motivation comprises reflective and automatic processes [18]. Behavior change experts have independently mapped the TDF domains onto the COM-B components, achieving unanimous consensus (Supplement 1) [18,20]. The COM-B system forms the foundation of the BCW, featuring nine intervention functions that address deficits in one or more of the COM-B conditions. Surrounding the BCW are seven policy categories that can support the implementation of these interventions [20]. Utilizing the COM-B system can assist in identifying which TDF domains are most relevant for modifying behavior. By beginning with such a behavioral analysis, intervention designers can selectively focus on the domains that will most effectively inform the development of the intervention [18].
Therefore, the objective of this study was to assess the extent of participation in and perceptions of antibiotic stewardship behaviors among nurses at children's hospitals. Additionally, the study aimed to gather nurses' perspectives on interventions for appropriate antibiotic use and to contribute to the development of strategies for establishing and disseminating antibiotic stewardship practices within healthcare facilities, particularly those focused on pediatric care.
METHODS
Ethics statement: This study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (No. H-2303-044-1410). Informed consent was obtained from all participants.
1. Study Design
This study was a descriptive research investigation focused on examining the perceptions of and participation in antibiotic stewardship among nurses in children's hospitals. The reporting of this study was based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [21].
2. Participants
The participants in this study were nurses employed at a single tertiary children's hospital in Seoul, Korea, who voluntarily consented to participate. The target population comprised all nurses working in the inpatient ward, intensive care unit, and emergency room of the hospital, excluding those who were newly hired or transferred during the orientation period. Nurses who met the inclusion criteria and were not subject to the exclusion criteria were deemed eligible for participation. The survey was distributed to a total of 150 individuals, and 125 participants ultimately agreed to and completed the survey.
3. Measurements
In this study, we utilized a tool previously employed by Chater et al. [22] to identify factors influencing nurses' participation in antibiotic stewardship behaviors. This tool was translated and back-translated following approval from the original tool developer, Angel Chater (a.chater@ucl.ac.uk), who granted permission via email. Initially, one researcher translated the original questionnaire into Korean. Another researcher then reviewed the Korean translation for accuracy and contextual appropriateness. Both researchers collaborated to consolidate their feedback and finalize the Korean version. An individual proficient in both English and Korean subsequently back-translated this final version into English. The back-translated questionnaire was compared with the original to ensure consistency in meaning. The comparison confirmed that the English and Korean versions conveyed the same meaning, affirming the suitability of the translated version for use. The questionnaire consisted of 61 questions in total, which included 9 questions on behaviors promoting responsible antibiotic use, 42 questions on influences affecting nurses' behaviors in antibiotic stewardship, and 10 questions on general characteristics.
1) General characteristics
The questions related to general characteristics covered a range of aspects, such as gender, age, educational level, clinical experience, nursing department, job title, experience with education on antibiotic stewardship, types of completed antibiotic stewardship education, the existence of a department dedicated to antibiotic management within the respondent's healthcare facility, and the identification of interventions deemed most effective in promoting the appropriate use of antibiotics.
2) Participation in antibiotic stewardship behaviors
The questions pertaining to behaviors that promote responsible antibiotic use were presented on a 7-point Likert scale. Respondents were asked to indicate the frequency with which they engage in these actions. The scale extends from “none of the time” (1 point) to “all of the time” (7 points), thereby gauging the degree to which these behaviors are practiced. A higher score signifies greater adherence to the behavior in question.
3) Perceptions of antibiotic stewardship behaviors
In this study, we assessed 14 factors that influence antibiotic stewardship behavior using the TDF. We further analyzed each factor by categorizing it into the three components suggested by the COM-B model as influencing behavior: capability (15 questions), opportunity (23 questions), and motivation (4 questions) [20,22]. We structured the questions about nurses’ perceptions of the factors that influence their antibiotic stewardship behaviors on a 7-point Likert scale. This scale ranged from “strongly disagree” (1 point) to “strongly agree” (7 points), with a higher score indicating a stronger agreement with the statement. We calculated the Cronbach’s alpha value to measure internal consistency and found it to be .947 in this study.
4. Data Collection
This study was approved by the Institutional Review Board (IRB). Following approval, we posted a recruitment notice for research participants in the nurses' ward or lounge, with the department head's consent. Interested individuals received a detailed explanation of the research, which clearly stated that there would be no repercussions for choosing not to participate. It also highlighted their right to discontinue the survey at any point. Participants who willingly chose to participate in the study expressed their consent by signing the questionnaire before beginning. After completing the questionnaire, they placed it in a paper envelope provided for this purpose, sealed it, and deposited it into a designated collection box. To maintain the confidentiality and anonymity of the responses, the researcher personally collected the sealed questionnaires from the box.
Participants who consented to the use of their personal information and provided their personal mobile phone numbers were compensated with a mobile gift card valued at 5,000 KRW upon completion of the survey. The survey required approximately 15 minutes to complete, and data collection occurred from April 11 to May 11, 2023.
5. Data Analysis
The collected data were analyzed using SPSS for Windows (version 20.0; IBM Corp.). Descriptive statistics were used to examine the general characteristics, the level of participation in antibiotic stewardship, and the factors that influence it. To investigate differences in the level of participation and the influencing factors in antibiotic stewardship based on general characteristics, a one-way analysis of variance was performed. When significant differences were found, the Scheffé test was applied for post hoc analysis. Pearson correlation coefficients were utilized to assess the relationship between the degree of antibiotic stewardship behaviors and the components of the COM-B model.
RESULTS
1. General Characteristics
The majority of participants (95.2%) were female, and 89.6% held a bachelor's degree. The average work experience among them was 86.7 months, with the most common job title being staff nurse, representing 93.6% of the group. The intensive care unit was the department where the largest proportion of participants (46.4%) worked, followed by the general ward (44.8%), and the emergency room (8.8%). A total of 16.8% of the participants reported having received training in antibiotic stewardship, with the vast majority (90.5%) indicating that they completed this training through continuing education programs. When asked if there was a dedicated department, team, or committee for antibiotic management, 60.8% answered “yes,” while 34.4% responded “don't know” (Table 1).
2. Antibiotic Stewardship Behaviors
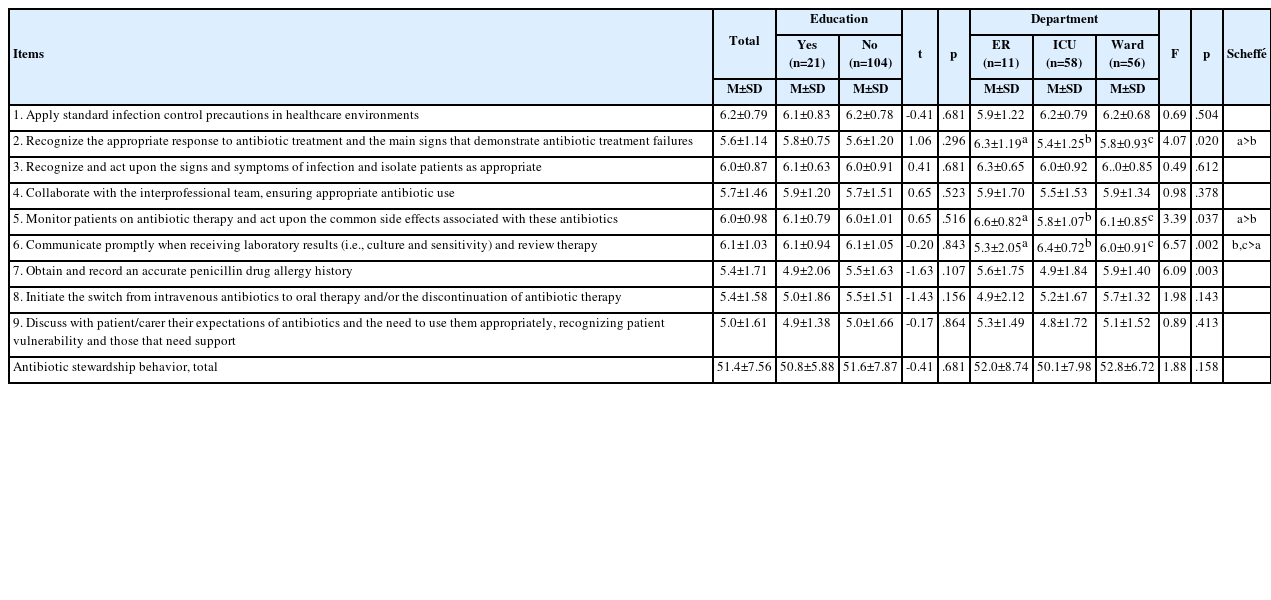
The highest level of performance for antibiotic stewardship was found for “apply standard infection control precautions in healthcare environments,” followed by “communicate promptly when receiving laboratory results (i.e., culture and sensitivity) and review therapy.” The lowest level of performance was found for “discuss with patient/carer their expectations of the antibiotics and the need to use them appropriately, recognizing patient vulnerability and those that need support” (Table 2).
3. Differences in Antibiotic Stewardship Behaviors Depending on Education Completion and Nursing Department
Antibiotic stewardship behaviors showed no significant difference based on education on the topic or the nursing department where the participant worked. However, a more detailed analysis revealed that specific behaviors exhibited statistically significant differences. These included “recognize the appropriate response to antibiotic treatment and the main signs that demonstrate antibiotic treatment failures” (p=.020), “monitor patients on antibiotic therapy and act upon the common side effects associated with these antibiotics” (p=.037), “communicate promptly when receiving laboratory results (i.e., culture and sensitivity) and review therapy” (p=.002), and “obtain and record an accurate penicillin drug allergy history” (p=.003), with variations depending on the nursing department (Table 2).
In the emergency room, the highest level of performance was found for “monitor patients on antibiotic therapy and act upon the common side effects associated with these antibiotics,” followed by “recognize the appropriate response to antibiotic treatment and the main signs that demonstrate antibiotic treatment failures,” and “recognize and act upon the signs and symptoms of infection and isolate patients as appropriate.” In the intensive care unit, the highest level of performance was found for “communicate promptly when receiving laboratory results (i.e., culture and sensitivity) and review therapy,” followed by “apply standard infection control precautions in healthcare environments,” and “recognize and act upon the signs and symptoms of infection and isolate patients as appropriate.” In the ward, the highest performance level was found for “apply standard infection control precautions in healthcare environments,” followed by “monitor patients on antibiotic therapy and act upon the common side effects associated with these antibiotics,” and “communicate promptly when receiving laboratory results (i.e., culture and sensitivity) and review therapy” (Table 2).
Conversely, in the emergency room, the lowest level of performance was observed for “initiate the switch from intravenous antibiotic to oral therapy and/or the discontinuation of antibiotic therapy.” In both the ward and intensive care unit, the lowest performance level was found for “discuss with patient/carer their expectations of antibiotics and the need to use them appropriately, recognizing patient vulnerability and those that need support” (Table 2).
The ward demonstrated a significantly higher likelihood of performing “obtain and record an accurate penicillin drug allergy history” than other nursing departments. The intensive care unit showed a greater likelihood of performing “communicate promptly when receiving laboratory results (i.e., culture and sensitivity) and review therapy” than other departments; however, the performance of “obtain and record an accurate penicillin drug allergy history,” “recognize the appropriate response to antibiotic treatment and the main signs that demonstrate antibiotic treatment failures,” and “monitor patients on antibiotic therapy and act upon the common side effects associated with these antibiotics” was lower.
The emergency room had a higher level of performance than the other nursing departments for “monitor patients on antibiotic therapy and act upon the common side effects associated with these antibiotics” and “recognize the appropriate response to antibiotic treatment and the main signs that demonstrate antibiotic treatment failures.” However, the performance of “communicate promptly when receiving laboratory results (i.e., culture and sensitivity) and review therapy” was lower (Table 2).
4. Differences in the Perceptions of Factors Influencing Antibiotic Stewardship Behaviors according to the Completion of Education
As a result of analyzing the perception of factors influencing antibiotic stewardship behaviors, divided into 14 factors based on the TDF, the highest level of recognition was observed for “beliefs about consequences,” followed by “social/professional role and identity,” and “skills,” with "optimism” also scoring high. The level of perception was lower for “environmental context and resources” and “memory, attention and decision-making” (Table 3).
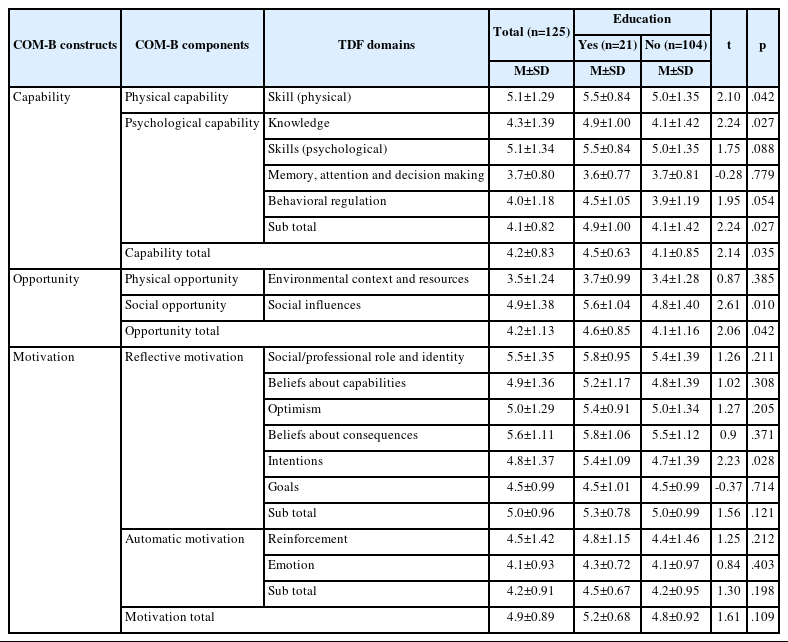
Differences between Theoretical Domains Framework Domains according to Education Experience about Antibiotic Stewardship (N=125)
When applying the COM-B model for further analysis, the scores for capability and opportunity were lower than those for motivation. Upon closer examination, the level of perception in the areas of “physical capability” and “reflective motivation” was high, whereas the level of perception in the areas of “physical opportunity” and “psychological capability” was lower (Table 3).
Comparing the level of perception by factors influencing antibiotic stewardship behaviors based on the completion of antibiotic stewardship education revealed significant differences in “skill (physical)” (p=.042), “knowledge” (p=.027), “intentions” (p=.028), and “social influences” (p=.010). When antibiotic stewardship education was completed, the levels of perception for “skill (physical),” “knowledge,” “intentions,” and “social influences” were higher (Table 3).
In the comparison of perception levels based on the sub-components of the COM-B model, significant differences were found in “physical capability” (p=.042), “psychological capability” (p=.027), and “social opportunity” (p=.010). The level of awareness of capability and social opportunity was higher when antibiotic stewardship education was completed than in other scenarios (Table 3).
5. Correlation between Antibiotic Stewardship Behaviors and COM-B Components
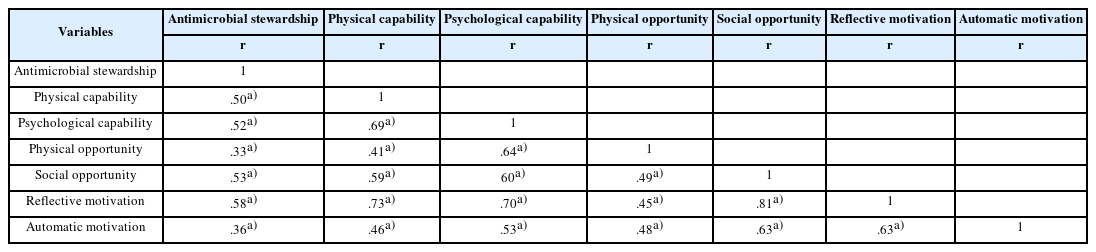
An analysis of the correlation between antibiotic stewardship behaviors and COM-B components revealed that all six components were significantly correlated with antibiotic stewardship behaviors (Table 4).
6. Opinions on Interventions to Improve the Proper Use of Antibiotics
When asked about interventions they believe would be most helpful in improving the proper use of antibiotics in their medical environment (multiple responses allowed), their responses were as follows, in descending order: “knowledge of accurate allergy reporting” (21.1%), “evaluation of antibiotics after 48 hours of therapy” (18.9%), “antibiotic restrictions” (17.8%), “pharmacy interventions” (12.4%), "lectures” (12.1%), “online education modules” (10.4%), and “auditing of charts” (7.3%) (Table 5).
DISCUSSION
In this study, we aimed to assess the extent of nurses’ participation in and perceptions of antibiotic stewardship in children’s hospitals. Our goal is to promote the involvement of nurses in the development of antibiotic stewardship programs within medical institutions and to encourage more proactive antibiotic management in actual healthcare settings.
In the implementation of antibiotic stewardship activities, tasks that were integrated into routine nursing duties and infection control education—such as compliance with standard precautions, prompt communication upon reviewing test results, recognition of signs and symptoms of infection, and appropriate isolation—demonstrated a higher level of performance. This was in contrast to activities that involved switching from intravenous antibiotics to oral therapy, discontinuing antibiotic use, obtaining a history of penicillin allergy, collaborating with the interprofessional team for appropriate antibiotic use, and discussing antibiotic expectations and proper usage with patients or carers. These findings are consistent with those reported by Chater et al. [22], who also found a lower level of performance in activities related to converting intravenous antibiotics to oral therapy, considering the discontinuation of antibiotic use, and engaging in discussions with patients or carers about antibiotic expectations and proper usage, as opposed to activities associated with standard precautions, recognizing symptoms of infection, and proper isolation.
In previous studies, it was discovered that many nurses were not familiar with the term “antibiotic stewardship,” despite being aware of their role in ensuring the appropriate and safe use of antibiotics for patients [16,23]. Furthermore, nurses' knowledge of antibiotic stewardship has been identified as lacking [12], which hinders their active participation in antibiotic stewardship programs [24]. A study by Ju et al. [25] that focused on Korean nurses revealed that only 75% agreed that nurses should be involved in interventions to improve antibiotic use, and there was a notable lack of awareness regarding the responsibility of nurses in the proper use of antibiotics. Consequently, it is crucial to develop a variety of strategies to bolster nurses' understanding of antibiotic stewardship and to clarify the specific and comprehensive roles they have within it, thereby encouraging their active involvement.
The level of antibiotic stewardship behaviors did not differ significantly based on whether individuals had completed antibiotic stewardship education. This absence of a significant difference could be due to the small proportion of respondents (16.8%) who had undergone such education. Although the analysis by nursing department revealed no statistically significant differences in overall performance, significant disparities were noted in responses to specific items. Therefore, it is essential to create education and intervention strategies that reflect variations in work characteristics and performance levels across various departments.
When asked about the presence of a department related to antibiotic management in their hospital, 49.2% of the nurses surveyed responded with “none” or “don't know.” This response indicates a significant lack of awareness among nurses about the existence and activities of their hospital's antibiotic management team. Furthermore, only 16.8% of the nurses reported having completed education in antibiotic stewardship, underscoring the need for broader and more robust educational initiatives to promote proper antibiotic use. Notably, the majority of those who had completed such education did so through continuing education programs. Given that continuing education is often available to only a limited number of participants, it is critical to provide a variety of educational opportunities related to antibiotic stewardship. This could include incorporating antibiotic stewardship topics into the existing in-hospital infection control education or creating and offering online educational modules.
The American Nurses Association and the CDC have recommended a deeper understanding of microbiology and pharmacology related to infections and drug therapy as a means to establish antibiotic stewardship [12]. Several previous studies have confirmed a positive correlation between providing antibiotic stewardship education and nurses' active participation in antibiotic stewardship programs [26]. These studies underscore the necessity of enhancing knowledge, education, and information provision in this area [27]. However, a survey of 217 Korean hospitals with more than 150 beds showed that only 14.3% offered regular education on the correct use of antibiotics. Among the hospitals that did provide such education, a mere 51.2% included medical personnel other than doctors [28]. Furthermore, a study involving 84 Korean hospitals with over 500 beds found that 60.7% of the respondents identified a lack of knowledge about antibiotic stewardship and infection control as an obstacle to collaborating with other departments for the appropriate use of antibiotics [29].
Hence, there is a need to develop educational content and broaden educational opportunities, encompassing pertinent knowledge, to integrate and implement antibiotic stewardship activities into routine nursing responsibilities. This should be coupled with an emphasis on the concept and significance of antibiotic stewardship, along with the roles nurses play in this context. Moreover, there was a notable demand for interventions such as “accurate allergy reporting” and “evaluating antibiotics after 48 hours” to increase the proper use of antibiotics. Identifying patient needs and incorporating the specific components of antibiotic stewardship into practical nursing activities and clinical settings will be of vital importance.
Upon analyzing factors that influenced perceptions of antibiotic stewardship activities, it was found that nurses generally viewed antibiotic stewardship as an important duty, responsibility, and mission. They also held optimistic and positive expectations toward these activities. However, awareness of support or networks for antibiotic stewardship was notably low, and there was a lack of focus on implementing such activities. This underscores the need for targeted education and the dissemination of information about antibiotic stewardship, with an emphasis on specific and practical applications. It is particularly concerning that 49.2% of respondents were unaware of the existence of their in-hospital antibiotic management team. This finding indicates the importance of actively informing nurses about the role and ongoing efforts of these teams within their institutions.
The study found a significant correlation between antibiotic stewardship behaviors and the components of the COM-B model, confirming the model's effectiveness as a theoretical framework for understanding behavioral changes. The COM-B model is valuable not only as an explanatory tool for behavioral changes but also as a basis for creating interventions to alter behavior [20]. Therefore, when utilizing this model for intervention design, it is crucial to clearly define the target behavior and determine which aspects of the behavior system must be modified to bring about the intended change [20].
The analysis of awareness regarding factors that influence antibiotic stewardship behaviors, based on the sub-components of the COM-B model, revealed relatively low awareness in the areas of physical opportunity and psychological capability. According to the COM-B model, these areas can be improved through environmental changes, knowledge transfer, and training in emotional, cognitive, and behavioral skills. This suggests intervention strategies such as education, training, environmental restructuring, and enablement to strengthen these components [20]. Furthermore, the study confirmed the effectiveness of education in improving the capability area, albeit to a limited degree. Given these findings, strategies to encourage nurses' participation in antibiotic stewardship behaviors should include initiatives such as intensified education and campaigns on antibiotic stewardship. These initiatives could leverage the expertise of in-hospital infection control teams, antibiotic management teams, and infection specialists. It is believed that the active involvement of these teams in educating staff about in-hospital antibiotic management activities and in developing intervention strategies will be more effective.
Furthermore, actively sharing information about the current status of antibiotic use, as well as antibiotic resistance rates both domestically and internationally, along with relevant data from medical institutions, can be advantageous. By disseminating this information through various channels, medical staff involved in patient care become aware of the existing issues and challenges associated with the proper use of antibiotics. Such transparency enables them to evaluate the effectiveness of antibiotic stewardship activities and serves as motivation for nurses to actively participate in these initiatives.
Antibiotic stewardship necessitates collaborative efforts from multiple disciplines, including doctors, nurses, and pharmacists. It is essential for professionals from various related fields to understand the concept and importance of antibiotic stewardship and to actively engage in its implementation. Nurses, in particular, are crucial to patient care workflows and communication, making them indispensable contributors to the successful execution of antibiotic stewardship initiatives. Therefore, it is vital to ensure that nurses receive ongoing education and training in antibiotic resistance and stewardship to equip them with the necessary knowledge and skills. Additionally, it is important to recognize nurses as integral to antibiotic stewardship activities at both institutional and governmental levels. Providing the necessary support ensures that nurses are aware of the significance of proper antibiotic use, enabling them to effectively carry out their roles in their daily practice.
This study has a limitation in that it was conducted among nurses at a single hospital. Therefore, the results must be interpreted and generalized with caution. Future research should aim to include larger samples from a variety of healthcare facilities. Based on the results of this study, we suggest a further study to develop strategies to improve nurses' participation in antibiotic stewardship and to evaluate their effectiveness.
CONCLUSION
This study aimed to assess the degree of participation in and perceptions of antibiotic stewardship among nurses at children's hospitals. There were several important findings. First, nurses demonstrated varying levels of participation in antibiotic stewardship activities, indicating a need for targeted education and interventions to address specific challenges. The study identified a low completion rate of antibiotic stewardship education among respondents, underscoring the necessity to expand educational opportunities. Additionally, a lack of awareness regarding antibiotic management teams within medical institutions was noted, emphasizing the need to better inform nurses about these essential resources.
Recognizing nurses as essential contributors to antibiotic stewardship, the study underscores the necessity for their active participation in initiatives that directly impact patient treatment. To empower nurses in this role, it is vital for them to understand the importance of proper antibiotic usage, which enhances the quality of medical care and ensures patient safety. Education tailored to the specific needs and practices of nurses is considered critical for developing this understanding. Furthermore, the study highlights the central role of nurses in patient monitoring, communication, and education, positioning them as key figures in promoting collaboration among various healthcare professionals for successful antibiotic stewardship. The findings indicate that future research should concentrate on creating strategies to strengthen the involvement of nurses in antibiotic stewardship efforts.
Notes
Authors' contribution
Conceptualization: all authors; Data collection, Formal analysis: all authors; Writing-original draft: all authors; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.
Supplementary material
The Theoretical Domains Framework Mapped to the Sub-component of the Capability, Opportunity, Motivation-Behavior (COM-B) Model