A systematic review and meta-analysis of studies on extended reality-based pediatric nursing simulation program development
Article information
Abstract
Purpose
This systematic literature review and meta-analysis explored extended reality (XR)-based pediatric nursing simulation programs and analyzed their effectiveness.
Methods
A literature search was conducted between May 1 and 30, 2022 in the following electronic databases: MEDLINE, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), and CINAHL. The search period was from 2000 to 2022. In total, 6,095 articles were reviewed according to the inclusion and exclusion criteria, and 14 articles were selected for the final content analysis and 10 for the meta-analysis. Data analysis was performed using descriptive statistics and the Comprehensive Meta- Analysis program.
Results
XR-based pediatric nursing simulation programs have increased since 2019. Studies using virtual reality with manikins or high-fidelity simulators were the most common, with six studies. The total effect size was statistically significant at 0.84 (95% confidence interval=0.50-1.19, z=4.82, p<.001).
Conclusion
Based on the findings, we suggest developing standardized guidelines for the operation of virtual pediatric nursing simulation education and practice. Simultaneously, the application of more sophisticated research designs for effect measurement and the combined applications of various virtual simulation methods are needed to validate the most effective simulation methodology.
INTRODUCTION
As we enter the era of the Fourth Industrial Revolution, the need for education that fosters complex problem-solving skills and convergent and creative thinking, as learners become subjects, has increased in the field of education [1]. In particular, the transition of the educational sphere to the digital generation has accelerated, leading to the rapid emergence of non-face-to-face class arrangements. For this reason and because of advances in information and communication technologies (ICTs), education sites are shifting away from traditional classroom methods and class designs are blending online and in-person learning activities. Furthermore, online platform-based remote lectures are gaining importance as an innovative model of education [2].
Extended reality (XR) is an innovative technology that has changed how humans understand and interact with digital information. The use of XR is expanding significantly through technological development and the accelerated digital transformation. Many attempts have recently been made to utilize the metaverse, which combines virtuality and reality, in education [3]. XR is an interface that connects reality and the virtual world, facilitating the coexistence of reality and virtuality and resolving the physical limitations of the real world [4]. In other words, technologies (virtual reality [VR], augmented reality [AR], mediated reality [MR], and hyper-reality) that enable communication via the realistic coexistence of the virtual world and reality maximize users' immersion, resolve the constraints of actual space, and connect and fuse virtuality and reality. As such, with the rapid development of these medical technologies and ICTs in recent years and the increasing severity and diversity of diseases, changes in nursing education are required to train future nurses who demonstrate these abilities related to ICTs.
Nurses are professionals who start working in the clinical field after graduation from nursing school. For them to acquire practical skills, both theoretical education and a certain amount of clinical practice are mandatory. However, the education of nursing students in the clinical field is limited, because most of it involves indirect rather than direct experiences in situations where patient rights and safety circumscribe the possibility of hands-on involvement. Specifically, because the field of pediatric nursing encompasses patients ranging from newborns to adolescents, the learning goal is to identify their health issues and to communicate and practice nursing appropriate for patients' developmental levels [5]. In 2020, South Korea's fertility rate was 0.84 [6], the lowest among the Organization for Economic Co-operation and Development countries. Clinical practice in the neonatal ward is challenging because of the low birth rate and risk of infection from infectious diseases such as coronavirus disease 2019 (COVID-19). In addition, despite the need to continue education in neonatal wards and involving high-risk newborns, it is difficult for students to have these experiences in person or make indirect observations as more hospitals scale down or close neonatal intensive care units. Regardless, realistic clinical sites are needed to provide educational opportunities for nursing students. An emerging alternative in this regard is simulation practice. Simulation exercises in South Korea have been prevalent since 2011. However, it remains challenging to implement vivid hands-on experiences in the nursing field as simulations despite extensive simulation exercises [7]. It seems necessary to develop a smart laboratory in which actual clinical practice can be conducted by combining virtuality and reality to strengthen the ability to materialize the actual clinical field in a simulation.
Most simulation exercises currently used in nursing programs are operated with scenarios developed by instructors as practice using simulators or standardized patients (SPs). The field of pediatric nursing mainly uses simulators because of the characteristics of its target patients. Recently introduced simulators are contributing to improving the quality of education, but their limitations include their high costs and inadequate realism for monitoring and other related situations [8]. Moreover, it is not possible to use simulations to attempt integrative nursing activities in the clinical field, where integrated thinking is required, because the scenarios are organized around diseases or symptoms. Instructors consider this educational method to be the most similar to the actual environment; however, it is unlike the actual environment from a learner's viewpoint and may lack the effect of learning immersion [9]. The realism of a simulation exercise is related to whether the targets are well-constructed and how faithfully the actual situation is reflected in the scenario [10]. Although some improvements are being made in the recently introduced high-fidelity simulators, the diverse and complex circumstances in the clinical field are not yet being reflected in an integrative manner. Improving these factors necessitates not only well-structured scenarios, but also a simulation environment that closely reflects clinical sites.
Considering these points, a simulation exercise model with a new platform of a smart environment that reflects academic characteristics and a changing environment is needed. To this end, it is necessary to identify the current status of simulations in nursing education, actively utilize the programs available for these purposes, and integrate these efforts. Although attempts are being made to use XR in the field of pediatric nursing [11,12], these attempts have been limited to building a smart environment and creating an integrated environment for nursing exercises based on these results. Therefore, this study aimed to systematically review studies on the development of XR-based pediatric nursing simulation programs, including AR, VR, and MR, assess the current situation in terms of development and effectiveness, and use the findings as a basis for building an environment for a pediatric nursing practicum using XR.
The aim of this study was to systematically review and meta-analyze research on the development of XR-based pediatric nursing simulation programs and assess the current status of their development, effectiveness, and limitations.
METHODS
Ethics statement: The Institutional Review Board (IRB) of the Gangneung- Wonju National University (GWNUIRB-R2022-24) reviewed this study. The committee decided that this study was an exempt research study.
1. Design
The present study is a systematic review and meta-analysis of the development and effectiveness of XR-based pediatric nursing simulation programs for nurses and nursing students. This study followed the criteria of the Preferred Reporting Items for Systematic reviews and Meta-Analyses 2020 (PRISMA 2020) checklist [13].
2. Key Questions and Selection Criteria
The participants, intervention, control, outcomes, and study design (PICO-SD) framework was used for this study, as follows: The participants of this study were nurses or nursing students who took part in studies of XR-based simulations for pediatric nursing. The interventions comprised XR-based simulations for pediatric nursing, and the control group and outcomes were not specified. The eligible study designs included randomized controlled trials, quasi-experimental studies, and similar designs. The inclusion criteria were as follows, and studies that did not meet the selection criteria were excluded:
Inclusion criteria
∙ XR application programs including VR, AR, and MR
∙ Programs applied to nurses or nursing students
∙ Studies that conducted an effectiveness analysis
∙ Studies that included interpretable and analyzable data
∙ Papers published since 2000
Exclusion criteria
∙ Studies that applied simple simulations not based on XR
∙ Studies whose participants were not nurses or nursing students
∙ Paper published in 1999 or earlier
∙ Dissertations or proceedings papers
3. Literature Review and Query Settings
The literature review and selection processes were performed according to the guidelines of the Cochrane Collaboration's PRISMA 2020.
1) Literature review
The primary search sources were electronic databases, namely MEDLINE, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL), and CINAHL. Google Scholar was also searched to procure as much gray literature as possible. The literature search was conducted from May 1 to 30, 2022, and the search period was set from the oldest publication year provided in each database to the date of the search in 2022.
2) Query settings
According to the PICO-SD parameters, the search term was "(nurse or nursing student or nurs*)" and "(reality or holo*) and (simulation) and (pediatric or child or children or baby or newborn or infant or kid*) and (RTC or trial* or experimen* or quasi or effect)".
4. Literature Selection Process
The literature selection was performed according to the PRISMA flow diagram, the results of which are shown in Figure 1.

PRISMA flow diagram of studies on XR-based pediatric nursing simulation programs. *Reason 1: If a simple simulation was applied, it was not based on extended reality or child nursing. Reason 2: Participants were not nurses or nursing college students. Reason 3: Studies on the evaluation of the process without an effect analysis. Reason 4: Studies that did not include interpretable and analytical data.
5. Literature Quality Assessment
The articles selected for the systematic review of this study were assessed for quality in each area of study design using the Risk or Bias and Risk of Bias in Non-randomized Studies of Interventions quality assessment tools. The areas assessed were as follows: the order of the random assignment, participants, assignment order concealment, levels of blinding of researchers, blinding of outcome assessments, selective reporting of insufficient results, and other sources of bias. Two researchers evaluated the quality assessments independently, and consistency was maintained after further discussion. In case of disagreement, a third researcher separately evaluated the quality assessments.
6. Literature Analysis Tools
The following details were identified and recorded by two researchers: authors, year of publication, country of study, study design, participant characteristics, sample size, type of XR program, scenario content, program operation and methods, outcome variables, measurement tools for the outcome variables, and experimental results. The experimental results correspond to the means, standard deviations, t-values, and p-values before and after the experiments.
7. Meta-analysis and Publication Bias Analysis
A meta-analysis was conducted to identify the effect size of the intervention using Comprehensive Meta-Analysis software. The effect size of variables whose homogeneity was not confirmed was calculated with a random-effects model that reset the weights considering the heterogeneity between the studies. The effect size was calculated by the standard mean difference value of individual studies [14]. The homogeneity of the selected studies was evaluated through the x2 and I2 tests. I2 values of 0% indicate no heterogeneity, 30% to 60% moderate heterogeneity, and 75% high heterogeneity [14]. Publication bias was assessed through an examination of a funnel plot and Duval and Tweedie's trim and fill [15].
RESULTS
1. General Characteristics
Regarding the years of publication, four studies were published in 2020, four in 2021, two in 2019, and one each in 2017 and 2016. The researcher's nationalities were as follows: six studies from the USA, six from South Korea, one from Canada, and one from Hong Kong. For research methods, a nonequivalent control group quasi-experimental study was the most common, used in five studies; followed by a methodological design in three; one-group pretest-posttest study in three; and a one-group posttest study, a mixedmethod study, and a retrospective method in one study each (Table 1).
2. Specific Contents
The XR type was identified as VR with manikin or high-fidelity simulation utilization in six studies [11,16-20], VR was used in four studies [21-24], AR in one study [25], VR and Hololens study [26] in one, a mixed-reality simulation using VR with SPs was conducted in one study [20], and realistic mock codes and team-based simulation training were implemented in one study [27]. Ng et al. [21] implemented virtual wards using 3D software and that allowed students to acquire injection skills and word dressing. Putnam et al. [26] trained students on pediatric airway management through VR using a Hololens (Table 1).
The target subjects of the programs were nursing students in seven studies [11,16,18,19,21,23,28] and experts, nurse practitioners, reviewers, and transport teams (including nurses) [17,20,24-27] in six studies.
Nine scenarios dealt with respiratory problems, including pediatric asthma, five focused on early neonatal care and neonatal intensive care, and there was one scenario each on pediatric sepsis, seizure, dressing and infection using a pediatric department and ward environment AR, and airway intubation using a VR airway.
The outcome variables that were used to evaluate the effectiveness of the XR programs included knowledge [16,18,19, 26,28], confidence (or self-efficacy) [18,19,25], competency (or performance or skills) [11,17,21,23,26], and critical thinking disposition (Table 1) [11,23].
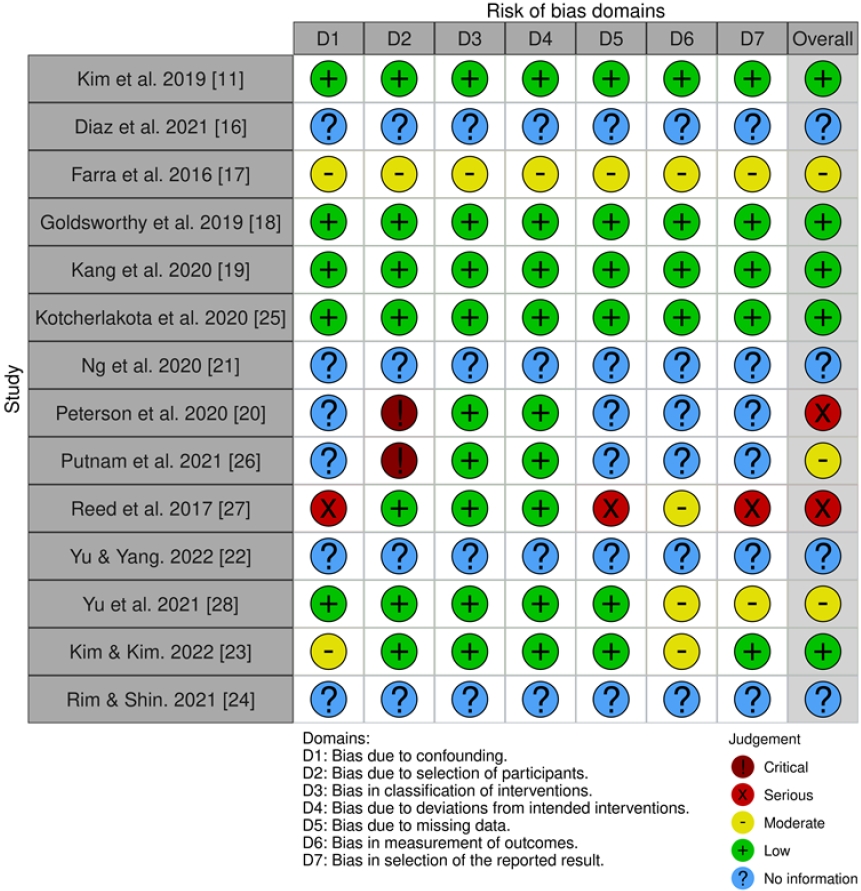
3. Quality Assessment of Studies
A quality assessment showed that five studies had a low risk of bias, three studies had a moderate risk of bias, two studies had a high risk of bias, and four studies had insufficient information to determine the risk of bias. Reed et al. [27] and Peterson et al. [20] conducted projects among experts working in a hospital, and there was a lack of an experimental design that would exclude confounding factors (Figure 2).
4. Effectiveness Analysis of Extended Reality-based Child Simulation Programs
In total, 10 studies were included in the meta-analysis, and the total effect size was statistically significant at 0.84 (95% confidence interval [CI]=0.50-1.19, z=4.82, p<.001) by using random effect. A study by Putnam et al. [26] had the largest effect size and the largest standard difference in means (3.08, 95% CI=2.37-3.78, z=8.49, p<.001). The I2 value in the heterogeneity evaluation of 10 studies was 82.0% (Figure 3). In a meta-analysis of nine studies, excluding that of Putnam et al. [26] due to high heterogeneity, the I2 value of heterogeneity was 0.00% and the pooled effect size was 0.60 (95% CI=0.47-0.74, z=8.57, p<.001) (Figure 4).
5. Publication Bias
Based on the funnel plots (Figures 3, 4), it was judged that there was no publication bias since the plots demonstrated a symmetrical form around the integrated estimate. Under a random-effects model, the point estimate for the combined studies was 0.84 (95% CI=0.50-1.19). Using Duval and Tweedie's trim and fill, these values are unchanged (Figure 3). Furthermore, under a fixed-effect model, the point estimate for the combined studies was 0.60 (95% CI=0.47-0.74). Using trim and fill, the imputed point estimate was 0.56 (95% CI=0.43-0.69) (Figure 4).
DISCUSSION
The spread of the COVID-19 pandemic has led to a paradigm shift in nursing education worldwide. In particular, the need for simulation-based learning tools has been increasingly emphasized in education on nursing techniques for newborns or children because of the need to protect children who are vulnerable to infection in pediatric nursing. Yu and Mann [29] reported that the use of VR programs, especially for infection control in high-risk neonates, was very effective both for improving practice skills and promoting problem-solving abilities. Our literature analysis showed an increasing trend in applications of VR and AR in pediatric nursing classes and exercises since 2019, along with increasingly many effectiveness analyses, and these trends reflect the social context and needs of educational sites. In particular, while simulations in the laboratory using manikin models were initially deployed in the early days of virtual simulations, the implementation of virtual simulations using online platform-based videos and images has expanded. In recent years, active efforts have been made to enhance realism through three-dimensional stereoscopic images using holograms or mixed VR and AR to provide learners with a realistic learning experience.
The literature analysis identified the following characteristics of simulations for pediatric nursing education and skills enhancement. First, the simulations had similar structures consisting of three components (pre-orientation, simulation run, and debriefing). Kim et al. [11] reported that the development and application of pediatric nursing asthma modules for nursing students with the abovementioned structure improved students' critical thinking, problem-solving, and competency. Goldsworthy et al. [18] also measured the effectiveness of a simulation on the same topic for nursing students, reporting a significant increase in clinical self-efficacy. Furthermore, many studies have induced learners to improve their knowledge through pre- and post-quizzes [21,24,28]. According to the results of these studies, the use of pre- and postquizzes improved learners' knowledge, critical thinking, and competency by reinforcing crucial learning content.
Regarding content, most studies dealt with serious conditions such as pediatric asthma, sepsis, neonatal seizure, infection, and apnea [11,16-18,23]. This is because nursing care for severely ill children at clinical sites requires high technical skills and knowledge in order to make accurate clinical judgments. Considerable risk is posed by the need for nursing students or novice nurses to gain practical experience in providing direct care to severely ill children. Therefore, replacing direct care with simulation nursing could make it possible to acquire the necessary competencies for providing nursing care to ill children while ensuring these children's safety.
In this regard, by applying XR simulations to child nursing education, experiential learning can complement theoretical learning content, enhancing the effectiveness of learning and contributing to the improvement of educational performance. A simulation session can also be organized as a team task for students in a child nursing course as an education support method that induces advanced learning through self-study and team discussion based on simulation cases. In clinical settings, simulations can be used to provide specialized education for nurses in children's wards, pediatric outpatient departments, and neonatal intensive care units. In particular, XR-based simulations developed for rare cases that are difficult to experience in the field or very severe conditions with high nursing difficulty can be used as an educational medium to improve nurses' professionalism and strengthen their practical capabilities.
Wide variation was evident in studies that applied simulations, ranging from research that applied three simulations, such as the studies of Diaz et al. [16] and Goldsworthy et al. [18], to those that applied 18 simulations, such as the study of Reed et al. [27]. The simulation time was mostly around 60 minutes, but there were differences between studies; for instance, the simulation lasted 150 minutes in the study of Rim and Shin [24]. The results of these studies indicate a need to develop standardized guidelines for the operation of virtual simulation education and exercises in pediatric nursing.
The overall quality of the literature included in this study was low, as shown by the fact that four studies had insufficient information for evaluating the risk of bias and two studies had serious concerns. This is similar to the results of the study of Kim and Kim [23], where the quality evaluation score of the literature included in the meta-analysis was found to be low, with an average of 5.61 points. Regarding this, Kim and Kim [30] reported that in a meta-analysis, research in nursing showed a similar level to that in dentistry and pharmacy, but nevertheless, few papers received relatively high quality scores. As a solution to this, it was suggested that academic societies need to update, disseminate, and encourage compliance with reporting guidelines for meta-analyses. Since the number of studies included in the content analysis and meta-analysis was very limited compared to the number of studies that appeared as search results, further analysis according to specific dependent variables or aspects of program operation was difficult. Therefore, it is suggested that a more sophisticated research methodology and research designs should be applied to study individual performance in order to expand the applicability of simulations to child care in the future.
It is expected that the transformation of educational methods that enable students to acquire advanced nursing skills without space and time constraints, especially for newborns and children who are vulnerable to nursing care, will accelerate in the future through virtual online exercises combined with innovative technologies such as VR, AR, and holograms. These advances make it possible to actively cope with sudden changes in the educational environment away from the traditional method of a practicum, which is centered on patient observation in hospitals. A prerequisite for this, however, will be a rigorous analysis and assessment of learning effectiveness. In that regard, several one-group posttest studies and onegroup pretest-posttest studies have been conducted, and there have been many attempts to conduct nonequivalent control group quasi-experimental research. Thus, it is necessary to evaluate the effectiveness of virtual online simulation education in pediatric nursing through the expansion of studies applying more sophisticated research designs, such as randomized controlled trials.
Virtual simulation education has many advantages, such as educational effectiveness, safety, and the absence of spacetime constraints. Investments should be made to cover the initial development costs, and a functional online platform must be developed in addition to simulated learning content. It is necessary to surmount various practical obstacles facing the field of education, such as the relatively short lifecycle of existing simulation programs because the technological development of online learning is evolving rapidly. This is a challenge to overcome for the expansion of virtual simulation education in pediatric nursing in the future. Furthermore, future research should examine the most cost-effective method of applying a mixture of virtual simulation methods, the effectiveness of which has been verified in prior research.
To date, researchers have attempted to develop and apply scenarios appropriate to their experiences and situations and to measure their effectiveness. However, we are moving toward an era where collaborative research is possible through online platforms that allow scholars to move beyond national boundaries, understand the difference between each other's cultures and institutions while interacting in the same space and time despite being physically located anywhere in the world, and create appropriate nursing models. Therefore, international standards for pediatric nursing simulation education should be formulated by conducting international collaborative research to develop, apply, and assess the effectiveness of scenarios. These initiatives will help design the most effective and efficient simulation education tools, contents, and methods for students of pediatric nursing.
CONCLUSION
The global COVID-19 pandemic triggered a dramatic shift in pediatric nursing education because newborns and pediatric patients (i.e., the subjects of pediatric nursing) are particularly vulnerable to infection and require a high level of competency and maturity in nursing education and care. Accordingly, the present study systematically analyzed research on applications of XR-based pediatric nursing simulation programs and assessed the effectiveness of the programs. The results showed that the incorporation of XR technology in the field of pediatric nursing is an advance from traditional patient observation-oriented education that ensures the safety of patients while simultaneously enhancing learners' nursing care capabilities. The development of pediatric nursing simulation programs combined with various virtual simulation technologies should be expanded in the future. We propose searching for pediatric nursing simulation methodologies that enable high effectiveness at a low cost. This search should consider key requirements, including the development of standardized guidelines for the operation of pediatric nursing virtual simulation education and practice, validation of the results of simulation studies through the application of sophisticated study designs for effectiveness measurement, and the combined application of various virtual simulation methods.
Notes
Authors' contribution
Conceptualization: all authors; Data collection, Formal analysis: all authors; Writing-original draft, Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
This study was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (No. NRF- 2021R1A2C1095530).
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.