Differences in the perceptions of partnership between nurses and mothers of children in a pediatric intensive care unit in South Korea: a qualitative study
Article information
Abstract
Purpose
The purpose of this study was to investigate how pediatric intensive care unit (PICU) nurses and the mothers of hospitalized children perceived their partnership and identify the detailed differences in the common domains of partnership between them.
Methods
A qualitative descriptive design with semi-structured and open-ended interviews was used. Interviews with mothers of hospitalized children and nurses in the PICU were conducted at a national university hospital in South Korea.
Results
Five integrated categories were identified concerning nurses' and mothers' perceptions of partnership. Five common domains were derived by merging the partnership categories perceived by each PICU mother and nurse: expectation of trust, sharing and communication, participation in care, equality in the relationship, and coordination of opinion However, there were significant differences in the composition of the categories of these common domains.
Conclusion
These results may facilitate more effective partnerships between parents and PICU nurses. Efforts should be taken to promote the formation of trust between nurses and parents and create an environment that is conductive to regular open communication in particular, steps should be taken to reduce gaps in awareness concerning this partnership and information sharing, nursing methods, and decision-making.
INTRODUCTION
Parents whose parental roles change when their child is admitted to an intensive care unit experience significant confusion [1,2]. The negative stress experienced by parents acts as a detrimental factor in the normal development of their children and affects their recovery from disease. However, the direct involvement of parents as caregivers has shown positive consequences on the health recovery of pediatric patients including shorter hospital stays, a lower risk of complications, reduced morbidity, and increased attachment [3,4]. Parental involvement refers to parents' active participation as direct care providers for their inpatient children.
In general, the pediatric intensive care unit (PICU) is an area within a hospital that specializes in critically ill patients, particularly infants, children, teenagers, and young adults. Complex technologies and equipment, especially mechanical ventilators and patient monitoring systems, are frequently used in the PICU [5]. Hospitalization of a child in a PICU is an emotional and stressful experience for parents because of the intensive care experience and constant monitoring [4]. Although PICUs retain many highly skilled medical personnel to care for children, it can be confusing for children not to know who everyone is or what everyone does.
The concept of partnership in the pediatric medicine can be defined as the process of communication and cooperation between parents and nurses for a common objective, which is the child's recovery [6], beginning with a relationship based on mutual respect, empathy, and support. The range of roles in a nurse-parent partnership should be determined through negotiation, with both parties assuming responsibility for their roles [7]. The relationship between parents and nurses should be perceived by both parties as an equal partnerships rather than a hierarchy in which one has higher or lower status than the other [6,8]. Nevertheless, a simple and unified definition of a partnership has not yet been established in this context. Rather, the concept of "partnership" is often ambiguous and abstract [9,10]. Mendes [10] reported various interpretive differences in the concept of partnership in a context where partnership was unambiguously need, in a study of parents and nurses using medical technologies such as tracheostomy, mechanical ventilation, intravenous infusions, or other medical technologies at home with the mutual goal of the child's recovery [10].
As the direct participation of parents increases, the importance of forming a partnership based on cooperation between parents and nurses also increase [8,10]. The use of the concept of partnership in pediatric medicine began after Casey [11] proposed "the partnership in care" model, which argued that the relationship between nurses and families is important for the care of children [11]. The concept of family-centered care also emphasizes participation and cooperation based on partnership between parents and nurses caring for children [8,10,12]. The nursing mutual partnership model of care focuses on how the partnership between nurses and parent educes parental stress [13,14].
In PICUs in South Korea, when children rely on medical devices on a long term basis, parents are encouraged to participate in care so that they can learn to effective caregivers both in the ward and at home [15]. Before the coronavirus disease 2019 (COVID-19) pandemic, the main activities of parents visiting the PICU included daily care (cleaning, feeding, and emotional support) and professional care (T-cannula suction, dressing, etc.) [15]. Regular visiting hours were observed, and additional time would be provided accounting to the discretion of the medical staff. This study examined the perception of partnership between medical personnel and parents, which is important to understand now that visits, which had previously been suspended due to the COVID-19 pandemic, are being reintroduced during the transition of COVID-19 to an endemic disease [15].
PICU nurses must provide encouragement and support to parents, as well as medical care for their children [16]. Encouragement is particularly important to mothers seeing their children during visiting hours. Furthermore, research conducted in contexts when parents' caregiving capabilities were restricted will help to further develop an academic understanding of the concept of partnership. Therefore, the purpose of this study was to investigate how PICU nurses and the mothers of hospitalized children perceived their partnership, and identify the detailed differences between them concerning common domains of partnership.
METHODS
Ethics statement: This study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (No. H- 1611-081-811). Informed consent was obtained from all participants.
This was a descriptive exploratory study using qualitative research methodology. Semi-structured and open-ended interviews were conducted to gain an in-depth understanding of the perception of partnership between mothers of children hospitalized in the PICU and nurses. A content analysis approach was used, as described by Field and Morse [17].
1. Settings
This was a single site study that recruited participants from a PICU at a children's hospital in South Korea.
2. Participants
The sample included mothers of hospitalized children in the PICU for more than seven days (n=7), and nurses who had worked in the PICU for more than two years (n=12). Semistructured and open-ended interviews were conducted between January and March 2017.
1) Mothers
Seven mothers whose children were hospitalized in the PICU, who spoke Korean as their native language, and who had sufficient ability to verbally describe their experiences participated in the study.
2) Nurses
Twelve PICU nurses who spoke Korean as their native language and had sufficient ability to verbally describe their experiences participated in this study.
3. Data Collection
The qualitative data collection methods in this study included individual interviews (face-to-face and telephone). We interviewed seven mothers and 12 nurses on a face-to-face basis between January 2 and March 25, 2017. Additional interviews were conducted to further explore the responses after analyzing the data, including a face-to-face interview with one of the mothers and telephone interviews with four of the nurses.
Prior to the interviews, all of the participants were informed that the interviews would be audio recorded for the purposes of data analysis, and their anonymity was guaranteed. The recorded content was transferred to a personal computer by one researcher and assigned a password. Interviews were conducted during participant-selected sessions in a quiet place to ensure the participants' privacy. A flexible approach to interview times was adopted to accommodate the nurses' shifts.
The interview questions were prepared based on a literature review by the investigators and included, questions on factors and attributes related to partnership [18,19] (Table 1). The interview guide by Ames et al. [20], who conducted interviews with parents about their' perceived role in PICU nursing, was also used to inform the interview design [20]. The interviews were conducted after obtaining IRB approval (IRB no. H- 1611-081-811). Permission for data collection was obtained from the tertiary hospital's nursing department and approve by all relevant department heads. One researcher oversaw the participant recruitment process. A notice was placed in the guardians' waiting room at the PICU with questions attached to identify mothers who were willing to participate. The same researcher posed a notice in the nurse's lounge of the PICU, where about 50 nurses worked, and contacted any nurses interested in participating to address any questions they raised. Consent forms were collected from participants after they were given an explanation of the purpose and procedures of the study. The consent form informed the participants of the purpose and content of the study (including that the interviews would be audio recorded) and guaranteed anonymity and confidentiality concerning the participants' personal details and responses. The form also informed participants of their right to cease participation at any time without any penalty.
4. Qualitative Data Analysis
Qualitative data analysis was carried out using the content analysis approach detailed in studies by Field and Morse [17], Guba and Lincoln [21]. This analysis method is based on a concept and theory that is extended through reinterpretation and reanalysis of newly acquired raw data. With the advice of a nursing professor with extensive experience in qualitative research on children and families, we attempted to highlights the relevance of content analysis in clinical practice. The content analysis approach states that the central premise of the inquiry must emerge from the researcher and recognizes that the interpretative significance of data sometimes requires the researcher to have courage and hold ideas tentatively until all pieces fall into place. Peer researchers should be debriefed about the meanings behind codes at an early stage of the analysis [21].
Field notes taken during the interviews were consulted to investigate the meanings and intentions of participants' responses in-depth. Next, the researchers extracted code and conceptualized meaningful statements by combining similar themes. Clusters of similar themes were grouped into categories and sub-categories. After the primary analysis was performed by the researcher who conducted the interviews, another researcher listened to the recorded interviews to confirm that participant's thoughts were reflected. If the researchers' opinions were inconsistent, an agreement was reached based on the advice of experts with experience in PICU work and qualitative research.
5. Evaluation of Validity and Rigor
The validity and rigor of the research outcomes were evaluated according to the criteria of Guba and Lincoln [21], which include credibility, confirmability, fitness, and auditability. The quality of representation depends on whether the research contains concrete descriptions, descriptions of a perceived or subjective experience, or descriptions of an interpretation of the experience. To ensure credibility and confirmability, bracketing was used to avoid the influence of any preconceived notions and minimize potential investigator bias. The fitness (applicability) of this study was confirmed by other PICU nurses and a professor of child nursing with extensive experience in research on children with chronic diseases who did not participate in the interviews for this study [21]. This study was confirmed to be applicable beyond the circumstances under which the results were obtained. To ensure auditability, the participants' interviews were transcribed, and researchers maintained a step-by-step sequence of the research process as it was conducted [21].
RESULTS
The mean age of the mothers of who participated in the interviews was 37 years. The mean age of the children hospitalized in the PICU was 14 months (8 months to 21 years), and their diagnoses included bronchopulmonary dysplasia, double outlet right ventricle, pulmonary hypertension, dilated cardiomyopathy, and respiratory distress syndrome. In addition, five out of the seven children had been hospitalized in the past, and the average length of their current hospitalization ranged from 8 to 360 days.
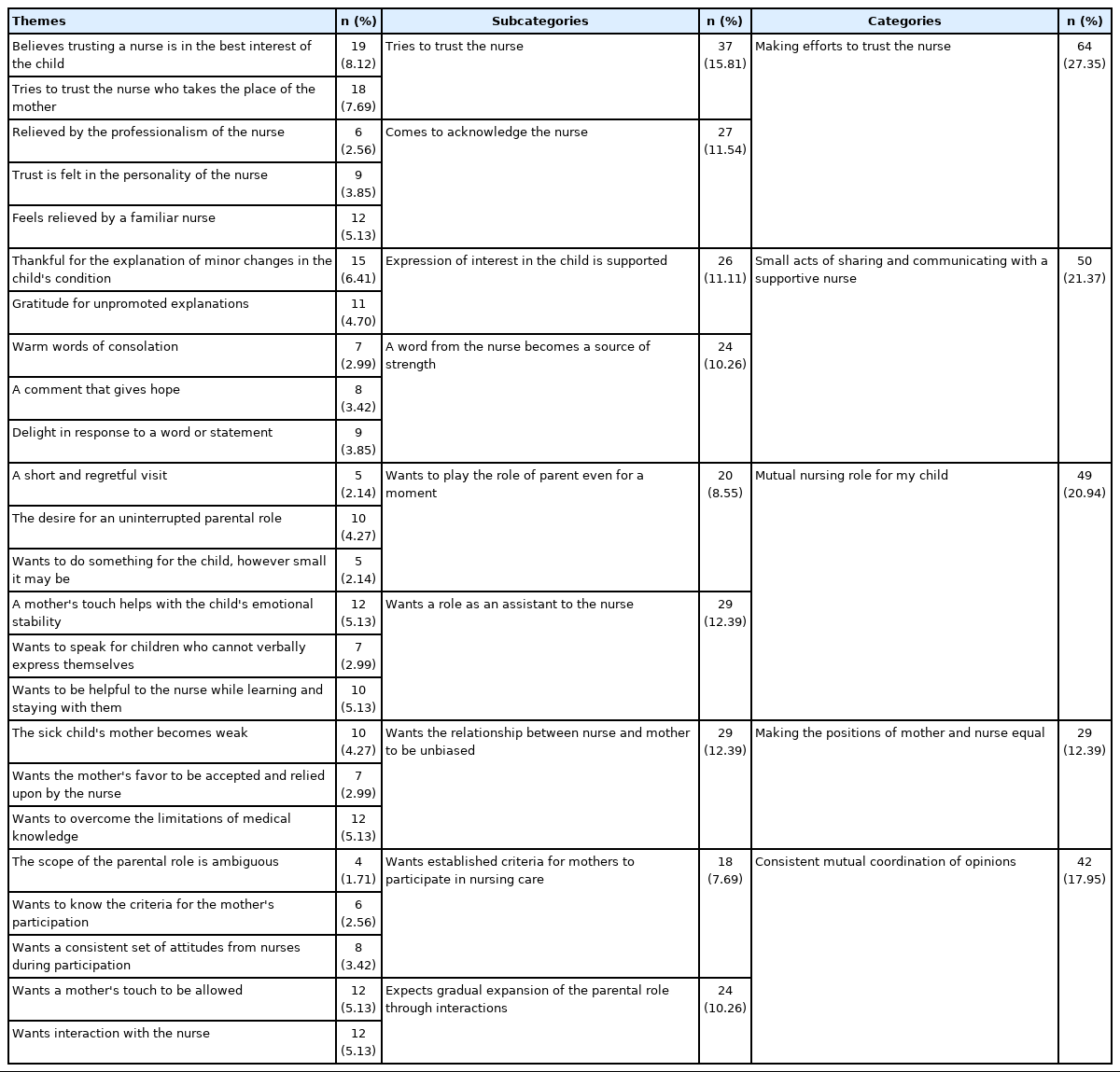
In the first step, specific themes were identified based on the results from the interviews with the mothers (Table 2) and nurses (Table 3) about their perceptions concerning of the partnership. Subcategories and categories were then derived by integrating common themes between mothers and nurses. In the second step, perceptions about the common domains of partnership between mothers and nurses were identified. Within each common domain, the researchers identified differences in the perceptions of mothers and nurses about partnership (Figure 1).
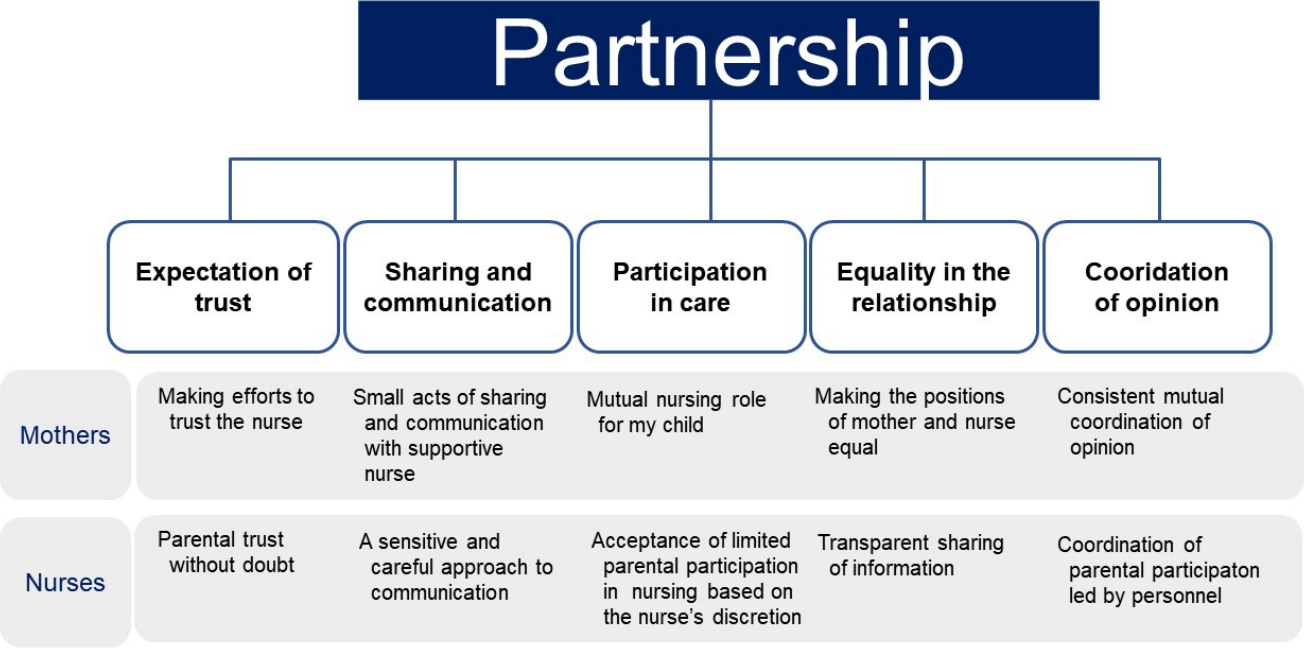
Differences in the perceptions of partnership between nurses and mothers of children in the pediatric intensive care unit.
1. Step 1: The Perceptions of Partnership
1) Part 1. The perceptions of mothers about partnership
Through interviews with seven mothers of children hospitalized in the PICU, 24 themes were derived and integrated into nine subcategories and five categories (Table 2). The five categories for which mothers perceived partnership were: "making efforts to trust the nurse", "small acts of sharing and communicating with a supportive nurse", "mutual nursing role for my child", "making the positions of mother and nurse equal" and "consistent mutual coordination of opinions". The mothers recognized that partnerships were enhanced of they trusted nurses and received minor updates about their children from nurses. The mothers believed that partnerships required nurses and mothers to care for the child equally rather than hierarchically and to regularly coordinate their opinions. These results reflect the feelings of regret experienced by mothers after their children are hospitalized in the PICU and removed from their care. Trust is the most important factor for mothers in the partnership between them and nurses. The mother must believe that the nurse who cares for her child during her absence is reliable. However, the belief in nurses is related to the child, and this can only be recognized gradually as the nurse talks about changes in the child.
At first, CPR was really hard. I was so sad. And then I became very emotional when you [the nurse] explained your face and felt sorry for me. I can't put it into words but I can see that it's all true. It's really supportive. (Mother A)
Thank you [to the nurse] for telling me what I didn't ask and paying attention to something you [the nurse] didn't even think about. (Mother F)
2) Part 2. The perceptions of nurses about partnership
In the interviews with 12 PICU nurses, 21 themes were identified and integrated into nine subcategories and five categories (Table 3). The five categories in which PICU nurses perceived partnership were: parental trust with no doubt, a sensitive and careful approach to communication, acceptance of limited parental participation in nursing based on the nurse's judgment, transparent sharing of information, and coordination of parental participation led by medical staff. The nurses believed that parents' unquestioned trust in PICU nurses when their role was limited formed the basis of the partnership. There is little that parents can do for their children in these situations, but the nurses believed that direct care provided by parents under the supervision of a nurse would help the emotional stability of child patients. However, owing to limited access, participation must be managed according to the discretion of the medical personnel.
A PICU is a place where visits are restricted, and if only parents are allowed, there could be a backlash. It's in the child's best interests to follow the judgement of nurses with regard to official requirements. (Nurse 1)
I think it's good for a mom to often show her face to her baby. A baby experiences a lot of anxiety when the nurse keeps changing in such an unfamiliar environment. I think a partnership is necessary so that nurses and moms can work together. (Nurse 8)
2. Step 2: Common Domains and Differences in the Perception of Partnerships between Mothers and Nurses
Five integrated common domains emerged after merging the categories of partnership perceived by each mother and nurse in the PICU (Figure 1).
1) Expectation of trust
Mothers whose children had been hospitalized in the PICU two or more times, or whose children had never been discharged from the PICU, experienced strong feelings of general anxiety. Their anxiety outweighed their trust due to the uncertainty of their children's recovery; they worried about possible exacerbation of the illness and about nurses caring for their children in their stead. Therefore, parents found hope and were encouraged by nurses who appeared comfortable and professional. They considered their trust in nurses to be central to the recovery of their children and made efforts to trust nurses.
I am not 100% satisfied, but at any rate, I think I have to trust the nurses because they are the ones who provide care for my child. When my anxiety increases, I cannot sleep or eat. Frankly, it is the thought of leaving my child with them. (Mother C)
PICU nurses wanted parents to be less anxious about their children's well-being and to trust them. They wanted mothers to believe that all of the nursing activities they undertook were with the child's best interests in mind expected mothers to have a positive attitudes toward the care of nurse.
It is a bit trite, but I think trust is most important. Mothers cannot stay in the intensive care unit 24 hours a day. They will be very anxious if they do not trust us since they are leaving their precious children with us. If I were the mother in this situation, I would feel the same way if I were not able to see my child. (Nurse 7)
2) Sharing and communication
Mothers who left their children in the PICU were concerned about their children's daily lives, such as how their children felt after being without their mothers for more than 20 hours. Mothers were thankful for information provided by nurses, especially when it was unprompted since it reflected a genuine interest in the child's welfare. Consequently, the mothers tended to ask the nurses who provided the most care about their children. The mothers were thankful for the information provided by nurses, especially when it was unprompted since it indicated to them genuine interest in the child's welfare. This information became a source of courage for mothers to gather the strength to get through the day.
I'm most grateful when you [the nurse] tell me this and that even though I didn't ask. Some nurses tell me that the baby prefers to lie on his left side;, unlike yesterday, he laughed a lot today;, it's warm, but his body temperature is fine. Thank you so much for saying these small things. (Mother F)
Conversely, nurses working in the PICU, whose first priority was to attend to serious medical issues, felt that delivering objective information about the child was their primary responsibility. For this reason, nurses were sensitive and cautious about delivering information to parents that could, have made them uncomfortable.
In fact, mothers want to hear a detailed and exact report from the nurse even if there "has been no change in the child's condition", but when they hear that the child's condition hasn't changed, they will ask again, "What's the same as yesterday?" even though they know the answer. What hurts parents most is when the nurse only states the facts. Rather than the test results, they wonder how the child spent the day. It is easy to understand when you think about it in numbers. "What did my child do for the past 24 hours…?" I don't know how to tell parents that the child's condition may deteriorate because it will make the parents sad. I am a bit hesitant as to how much I, as a nurse, have to explain on behalf of the doctor. (Nurse 8)
3) Participation in care
Mothers who were cut off from their parental role wanted to be on their child's side, even if only for a moment. They believed that a mother's touch would give their children emotional stability and wanted to gain nursing knowledge while in the presence of their children.
Since nurses are professionals, I would like them to be in charge of critical procedures such as suction. I will be an assistant. I will help with such things as changing diapers, giving the baby a bottle, and changing the linen while learning from the nurse about things such as suction. (Mother C)
However, the role of nurses differed. While a mother's touch can offer comfort, some children require prompt medical treatment from nurses and doctors. Nurses in the PICU who found themselves in such situations worried that the parents' presence during an emergency may be distracting.
A mother's participation in nursing is optional, not a requirement. We can do it without their participation, so it is not essential. (Nurse 6)
A mother's participation should be determined by the characteristics or condition of the patient. If the child is in a fair condition, the child can be taken care of by the mother and the child also often wants his or her mother. Also, children with "Do Not Resuscitate" orders need their mothers. The nurse's judgment is important, however, since even parents who are not allowed to participate want to participate. (Nurse 9)
4) Equality in the relationship
Neither mothers nor nurses considered themselves to have an equal relationship. The role of mothers diminished simply because they had to leave their sick children in the PICU. A Mothers who could not do much for their children requested that the nurses pay more attention to the child.
It is not an equal relationship since we leave our children under their care. Because we are still asking for a favor even though we pay for their services, and we feel that if we do something wrong, it could be bad for our child. We don't think it is an equal relationship. We always ask the staff to take good care of our children. (Mother F)
Similarly, nurses believed that the relationship could not be equal since medical personnel have more medical knowledge, which is more important for the child's welfare in a hospital context.
That's because these children are sick. When the child is admitted into the pediatric intensive care unit, parental rights are cut off. They can only see their children at a set time and only listen to decided matters. (Nurse 3)
5) Coordination of opinions
To form a partnership in the PICU, participation beyond that of regular visiting hours is required. For this to occur, differences in opinions should be coordinated at the outset, when nurses and mothers are still unfamiliar with one another. The interviewed mothers believed that consistent mutual coordination of opinions should be undertaken in the process of determining criteria for participation in nursing.
When I came here the first time, I felt like there was an invisible wall between the nurses and parents. I think meetings are necessary, even if they are once a month. (Mother A)
However, the nurses believed that parents should accept decisions made by medical personnel based on the medical institution's policies.
It is necessary to be consistent regarding your respective roles without overstepping any boundaries. Sometimes, mothers go beyond nurses' boundaries. For example, when the syringe is empty, mothers sometimes turn off the syringe pump and turn on the three way. That is really scary. It is very embarrassing when they expand their roles into our area. It is important to maintain boundaries. (Nurse 7)
DISCUSSION
Most studies on nursing partnerships to date have been limited in their understanding how of perceptions of mothers, children's primary caregivers, about the nurse-parent partnership since previous research has mainly focused on the perceptions of nurses about this partnership, covering the perspective of medical personnel only. Moreover, most studies have been conducted in general wards, neonatal intensive care units, and contexts in which parents could care for their children directly [22,23].
Moreover, the perceived meaning of the term "partnership" can differ depending on the situation and context. This study was therefore conducted to shed further light on the gap between parents and nurses concerning partnership. The results of this study revealed that there were differences in the recognition of the nurse partnership, as well as in the most important factors for strengthening the partnership between mothers and PICU. Accordingly, understanding and respecting the perceptions of the partnership between mothers of hospitalized children and nurses is essential for a successful partnership between. Common domains related to the partnership between mothers and PICU nurses were also identified.
In this study, the primary differences concerning the perception of the partnership between medical personnel and parents were as follows. Mothers and nurses both recognized that their partnership benefited the physical and mental recovery of critical patients, but their perceptions also differed. The mothers wanted to learn from nurses about the small differences between the child's appearance at home and procced together by sharing their insights and observations with the nurse. However, the nurses had other ideas about their role as nurses, and their emotions were more limited to the task of sharing opportunities for mothers to participate in care and provide information to parents when they were not with the child.
Trust was the most frequently cited concept in previous studies investigating the attributes of partnership [9,18]. The finding that trust is important to both mothers and nurses is consistent with those of previous studies [10,18]; however, the finer details of participants' perceptions of trust differed in this study. For parents whose anxiety level is high due to uncertainty about their child's recovery and who are isolated from their child's treatment, trust is essential. The statement by one mother from this study who cited drawbacks of not trusting nurses indicates that the mothers indeed wanted to trust the nurses. In other words, mothers can be said to have made a conscious effort to trust the nurses. However, nurses want parents to trust them so that they are not suspicious of their caregiving ability. Therefore, if medical personnel want parents to understand and comply with nurses' opinions and guidance without doubt communicating their thoughts and opinions more openly will contribute to promoting a strong nurse-parent partnerships [18].
Information sharing was found to be important for partnerships in family-centered nursing. Specifically, sharing trivial information about the child between mothers and nurses was essential for developing efficient and coordinated communication while caring for pediatric patents. However, there were also communication difficulties from the perspective of PICU nurses. Nurses were cautious about how and how much information to share about the child, especially in circumstances when the child's condition was unstable or constantly changing.
Parents expect their participation in care for their child to positively influence the formation of a partnership with the nurse in charge. Nurses, however, believe that the level of participation should depend on their assessment of the situation. Blankenship et al. [9] revealed that parents' regular participation in the PICU care of their child also helps the child's emotional stability [24]. Rather than worrying because they did not know the child's condition from outside the ward, they understood the situation better by providing some care for the child through personal participation. In other words, the uncertainty and anxiety of parents were reduced, which positively affected their children, contributing to patients' psychological stability. However, the study also noted that an expansion of the parental role in the PICU could pose ongoing challenges in the future.
Mothers of hospitalized children by default occupy a secondary position to that of nurses when it comes to the child's care. For mothers who feel that nurses have more power over the situation, references to an equal relationship can be interpreted as a desire for an unbiased distribution of power in the relationship and an equal position between mothers and nurses. Nurses also recognized the formation of unequal relationships due to their greater medical knowledge regarding the child's condition. Therefore, bidirectional decision making that includes parents is necessary when determining the direction of treatment for child patients. Since the sense of equality in a relationship can be subjective or fragmented and based on emotions, research on changes in the perception of equality throughout the course of a patient's illness, as well as after treatment has ended, is recommended.
Even when parental participation in nursing is possible, there are still barriers when parents must take on an unfamiliar role. Therefore, obtaining nurses' opinions on the role of parents is essential [24]. Ideally, all concerned parties should be involved when selecting criteria for parental participation in nursing so that all stakeholders can understand the expectations and, processes involved. However, our results showed that PICU nurses also preferred to establish criteria for parental participation, including objective criteria concerning participation time, and they believed that the coordination of opinions should be led by medical personnel. They felt that the development of objective criteria could prevent conflict between parents and nurses.
Furthermore, when the criteria for parental participation in childcare are unclear, it can lead to confusion among parents, further increasing the conflict between caregivers and medical personnel. In addition, the medical personnel at the PICU where the study was conducted agreed that family care, such as emotional support for family members was although important difficult to maintain [25]. Based on the results of this study, the perceptions of each party about partnership should be understood at start of family-centered care since, partnership may be difficult in the context of family nursing in the PICU. After Casey [13] proposed the partnership in care model, the term "partnership" has been used in care for children, which is considered a component of family-oriented care. This led to the development of the family partnership model within the family sector, which highlights the inclusion of parents in the care of child patients [13,26].
The findings of this study, which identified five integrated common domains, suggest that a strategy for promoting partnership in PICUs can be divided into three parts. First, PICU nurses and mothers should participate in direct and in-depth communication with a professional attitude to build trust. Rather than brief meetings, in-depth communication is needed. Second, to work together as facilitators of a pediatric patient's care, both parents and nurses should be given carefully defined roles. Finally, this partnership should be strengthened by repeated coordination of opinions, rather than doing so once.
Some limitations should be considered before applying this study's findings in pediatric practice. Mothers of hospitalized children were the focus of the current study; therefore, the findings cannot simply be interpreted more broadly to include the perceptions of fathers. In addition, this study was conducted at a PICU in the largest national hospital in South Korea. The regular intensive care unit also contains children hospitalized for other medical problems, whereas the PICU specifically offers acute surgical care. Therefore, this study was limited to identifying differences in the perception of partnership among mothers of children with medical problems requiring acute surgical care.
CONCLUSION
Using content analysis, the perceptions of mothers of children hospitalized in the PICU and nurses were analyzed to identify areas of common understanding regarding the topic of partnership. Five common domains were identified in the analysis as components of partnership: expectation of trust, sharing and communication, participation in care, equality in the relationship, and coordination of opinions. Despite the emergence of integrated domains of partnership, differences between the perceptions of mothers and nurses were confirmed. The most meaningful difference in the perception of the parent-nurse partnerships was that parents wanted equal partnerships with nurses, whereas nurses preferred a strong, nurse-led partnership.
These common, integrated themes suggest the following partnership-promoting strategy for PICUs, where parental visits are restricted: building trust through confidence, communicating in-depth with a professional attitude, delegating clearly-defined roles to both parties, and coordinating opinions on a repeated rather than one-off basis.
The five common domains and categories identified in this study highlight the most relevant topics to promoting a strong partnership, which is a key factor in family-centered nursing, between mothers and PICU nurses. These domains are expected to be used as a framework for developing effective strategies and policies to facilitate trust and create an environment for regular and open communication to promote partnership through parental participation in PICU care.
Notes
Authors' contribution
Conceptualization: all authors; Data collection: Bobae Park; Formal analysis: all authors; Writing-original draft, Writingreview and editing: all authors; Final approval of the published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.