The association between the social adaptive skills of school-aged children with congenital heart disease and mothers' decision factors for providing disease explanations in Japan: a cross-sectional study
Article information
Abstract
Purpose
This study aimed to clarify the factors related to mothers' decisions to provide disease explanations to their children, investigate the associations between those factors and social adaptive skills, and examine support relative to children's growth and development.
Methods
Data were collected from anonymous, self-administered questionnaires answered by 71 mothers of outpatient school-aged children with congenital heart disease. The questionnaire items included characteristics of mothers and children, decision factors for providing disease explanations, and children's social adaptive skills (Asahide-Shiki social adaptive skills test). Factor analysis was performed on the decision factors, and multiple regression analysis was performed to examine the association between the identified factors and each social adaptive skill.
Results
The decision factors for providing disease explanations were the mother's explanation ability, the receptive capability of the child, and the child's interest and literacy regarding the explanation. Multiple regression analysis showed that language and social life skills were significantly associated with the child's receptive capability, and language and daily life skills were significantly associated with the child's interest and literacy regarding the explanation.
Conclusion
Improving children's language, social life, and daily life skills may enhance their receptive capability and literacy regarding explanations of their disease.
INTRODUCTION
Congenital heart disease (CHD) is generally life-threatening and often requires surgery; however, the treatment of CHD has improved in recent years. Patients with CHD born between 1990 and 1993 reportedly had a cumulative mortality rate of 4% at the age of 18 years [1]. Moreover, children with more complex forms of the disease have a health-related quality of life 17% lower than that of the general population [2,3]. Even children with milder forms of CHD may experience serious health and lifestyle limitations [2]. Therefore, children with CHD, regardless of its severity, face various challenges in their social lives, which require a process of understanding, accepting, and adapting to their disease.
However, children with CHD often do not have a good understanding of the disease. Patients demonstrated a poor level of knowledge on all five thematic subscales (knowledge about CHD diagnosis, cardiovascular risk factors, symptoms of deterioration, endocarditis, and reproductive issues) [4], and other studies have consistently reported additional inadequacies [5-7]. Furthermore, young patients relied more on the information provided by their parents than on the information provided by their doctors [8], and the people who explained the disease for the first and subsequent times were reported to be "parents," "doctors," and "parents and doctors" in that order [9]. These suggest that mothers play an important role in providing information to their children. A previous study by the present authors found that since the explanations given by mothers to their school-aged children about their disease consisted of daily life tips along with imperfect medical information [10], it is imperative to examine disease explanations, especially explanations that stem from insufficient medical information.
Additionally, school-age children are at a psychological developmental stage of industry versus inferiority, which is very decisive stage from a social standpoint [11], as children learn through education and gain the necessary experiences for social interaction with their friends and adults. Therefore, the ability to adapt to their expanding social context, including intellectual ability, plays an important role in the growth and development of school-aged children; however, children with CHD have significantly more problems with motor functioning, autonomy, and cognitive functioning than their counterparts [12]. Thus, the ability to adapt to the expansion of children's social context, including intellectual ability, is even more relevant for children with CHD. Since mothers provide disease explanations for their children's as they grow up, an association would be expected to exist between children's social adaptive skills and the factors related to mothers' decisions to provide disease explanations. However, no studies have examined this association or developed a measure to evaluate the factors that contribute to mothers' decisions to provide disease explanations to children.
The first aim of this study was to clarify the structure of factors contributing to mothers' decisions to provide disease explanations to their children with CHD. The second aim was to clarify the association between the social adaptive skills of school-aged children with CHD and the decision factors for mothers' provision of disease explanations, focusing on insufficient medical information. The findings will help provide support for improving explanations containing insufficient medical information, in accordance with children's growth and development.
METHODS
Ethics statement: This study was approved by the Research Ethics Committee of the Nagoya City University (No. 19026) and the Medical Research Ethics Review Committee of Nagoya City University Hospital (No. 60-19-0192). All participants agreed to participate in the study.
1. Study Design
This cross-sectional study used data collected from anonymous self-administered questionnaires.
2. Participants
We included mothers of school-aged children (6-12 years old) with CHD who did not have problems with intellectual development, and the data were collected from March to August 2020. At the outpatient clinic of the department of pediatrics at Hospital A in Japan, we received a list of patients scheduled to be examined by nurses based on the target age group; the decision to include a patient in the study was made after confirming the child's intellectual development with the attending physician.
Participants were provided written and oral explanations of the study and were handed a paper questionnaire form. The completed paper questionnaire forms were collected by mail. We requested 94 people to participate in the survey, distributed questionnaires to 87 people who agreed to take part, and collected questionnaires from 73 people (response rate: 83.9%). Valid responses were obtained from 71 respondents. The number of participants was determined from the minimum sample size required for statistical analysis. Exploratory factor analysis requires a sample size of at least 5 to 10 times the number of items [13].
3. Measurements
The questionnaire contained items on the characteristics of the mothers, children, and the disease, children's social adaptive skills, and the decision factors for providing disease explanations.
1) Social adaptive skills
The Asahide-Shiki Social Adaptive (ASA) skills test was developed by the Asahide-Gakuen Educational Research Institute after thorough validity and reliability studies [14]. This measure is used to measure children's social adjustment skills. This test is suitable for children of all ages, from kindergarten to high school, and can be administered by people who know the child well, such as parents or homeroom teachers. It consists of language skills (skills related to basic language understanding and expression and reading and writing skills), with nine subdomains (57 items); daily life skills (skills necessary for living at home), with five subdomains (31 items); social life skills (skills necessary for living outside the home and in the community), with nine subdomains (49 items/52 items for junior high school students and above); and interpersonal skills (skills necessary for interpersonal interaction and group participation), with nine subdomains (52 items). The responses consist of two or three options. Items with two choices are scored as 0 or 2, and those with three options are scored as 0, 1, or 2. (0: cannot do it, have never done it; 2: can do it, do not do it now, but used to do it when the child was younger; and 1: a middle rating set for some items). The total score is calculated by adding the scores for each subdomain or skill. By matching each skill score to the "Skill Score to Equivalent Age Conversion Table", we could evaluate each skill in terms of the child's equivalent age. This tool is particularly useful for the educational assessment of children who are struggling with the skills necessary for social adjustment or children who require some form of support; children without intellectual disabilities are also included.
2) Decision factors for providing disease explanations
We assumed that decision factors contribute to mothers' choice to provide disease explanations to their children, and that when more of these decision factors apply, mothers will be more likely to provide explanations. Question items corresponding to these factors were adopted from a previous study by the present authors. There were 19 items, 18 of which were developed in a previous study [10] based on the "factors of information selection that increase and expand with the child's growth and development," and one item was based on the mother's understanding of the child's disease. The items were constructed so that the current situation could be assessed through past experiences using a 6-point scale (1: strongly disagree to 6: strongly agree) for each item.
4. Data Analyses
SPSS version 22 (IBM Corp., Armonk, NY, USA) was used for the analysis, and the significance level for each test was set at p<.050. The collected data were analyzed using descriptive statistics, multiple regression, and exploratory factor analysis.
The constructs were extracted from exploratory factor analysis of 19 decision factors for providing disease explanations, and their reliability was examined. The principal factor method and Promax rotation were used for extraction, and the number of factors was determined by scree plots, eigenvalues greater than 1.0, and the cumulative contribution before rotation. Items with factor loads of at least 0.4 were selected for interpretability. Items that had ceiling and floor effects were removed.
Next, multiple regression analysis (using the forced-entry method) was performed using the total score of each item for the degree of the extracted factors as the objective variable and the children's social adaptive skill scores and confounding factors as explanatory variables. The social adaptive skills were analyzed separately, considering the influence of skills on each other. The confounding factors were the child's age and sex (male/female) as general confounding factors, current self-care needs (limited exercise and oral medication vs. no need for either or both) as factors directly linked to disease explanations, and the mother's education (high school graduate or less vs. vocational school or college graduate or more) as a factor likely to influence maternal disease understanding [15]. Multicollinearity was evaluated by calculating the variance inflation factor (VIF) for each independent variable. Multicollinearity was determined to have occurred when the VIF was higher than 10. Serial correlations were checked based on a Durbin-Watson ratio of 2.
5. Ethical Considerations
After obtaining approval from the Research Ethics Committee of the authors' institution (No. 19026) and the Medical Research Ethics Review Committee of Hospital A (No. 60-19-0192) in Japan, we obtained permission from the head of the pediatric department, the attending physician, nursing department, and head of the outpatient nurses. In a private room, research participants were informed of the purpose, content, and methods of the study, as well as of the protection of anonymity. The participants were given the option of participating and discontinuing participation, along with the reassurance that there would be no repercussions if they refused, and they were clearly informed that completing the questionnaire would be considered providing consent to participate in the study. Additionally, because the ASA skills test uses the same questionnaire items for all children, from infants to high school students, and because the questionnaire includes some items that can be naturally answered by schoolchildren and items that can excessively underestimate children's development, a sufficient explanation was given. As a reward, we gave participants a 500-yen gift card.
RESULTS
1. Characteristics of Participants and Their Children
The mothers' mean age was 42.0 (standard deviation [SD]= 5.1) years, and 48 (67.6%) had at least technical school/college graduation as their highest degree of education. The average age of their children was 9.7 (SD=1.8) years; 42 (59.2%) were boys. The most common CHD diagnosis was ventricular septal defect in 29 (40.9%) children, followed by double outlet right ventricle in seven (9.9%). Fifty-four (76.1%) children were still taking medications, and 11 (15.5%) had exercise restrictions of grade D (moderate exercise allowed) or higher on school life guidance forms. Sixty-three (88.8%) children had siblings (Table 1).
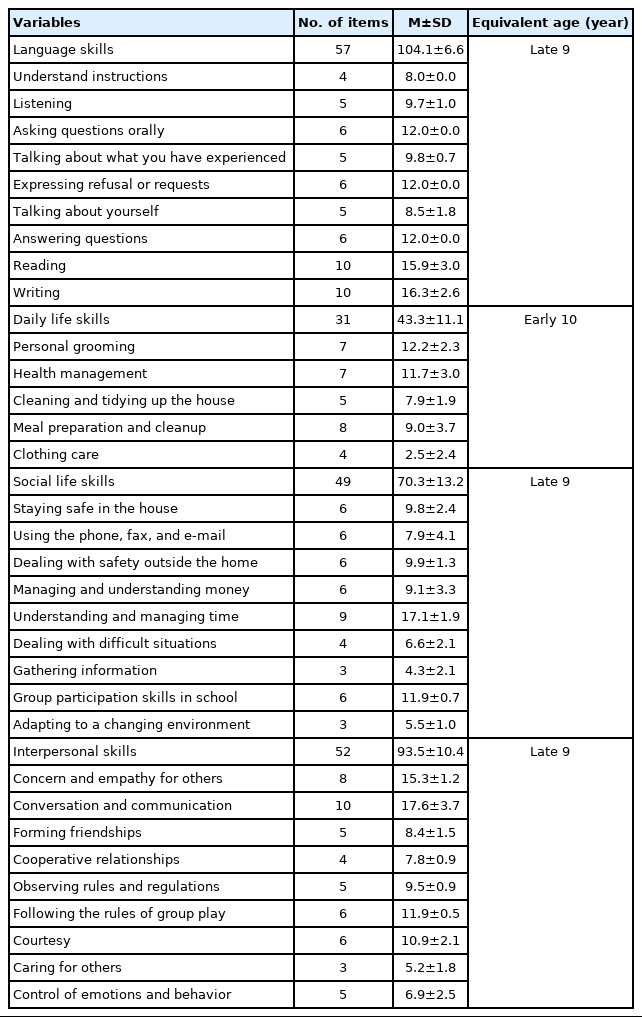
2. Children's Social Adaptive Skills
The average score for language skills was 104.1±6.6 points, equivalent to that of a late 9-year-old; the average score for daily life skills was 43.3±11.1 points, equivalent to that of an early 10-year-old; the average score for social life skills was 70.3±13.2 points, equivalent to that of a late 9-year-old; and the average score for interpersonal skills was 93.5±10.4 points, equivalent to that of a late 9-year-old (Table 2).
3. Factor Structure and Subscale Scores of Decision Factors for Mothers' Provision of Disease Explanations to Children with Congenital Heart Disease
Nine of the 19 items received a positive evaluation, ranging from 4 ("slightly agree") to 6 ("strongly agree"), from more than 70% of the respondents (Table 3).

Distribution of Responses to Decision Factors for Mothers' Provision of Disease Explanations to Children with Congenital Heart Disease (N=71)
Since item 18 had a ceiling effect and items 14 and 15 had a floor effect, they were excluded, and factor analysis was conducted on the remaining 16 items. Two patients had missing responses for the decision factors for providing disease explanations. One patient was excluded from the analysis because he was missing nine items, and another was included in the analysis despite missing two items, because those items were excluded from the analysis due to the floor effect. During the analysis, four items (items 4, 5, 9, and 19) were deleted, and 12 items were extracted as three factors. In the factor analysis, the Cronbach's α coefficients were .815 for all 12 items and .709-.796 for each factor; the cumulative contribution ratio was 62.94%(Table 4).

Factor Structure of Decision Factors for Mothers' Provision of Disease Explanations to Children with Congenital Heart Disease (N=70)
The first factor was named "the mother's ability to communicate an explanation" and consisted of four items: "2. You have the eloquence to explain medical information to your child", "1. You understand the medical information related to your child's disease", "17. You have a relationship with your child where you can explain medical information", and "3. You have resources (e.g., explanatory documents and picture books) for explaining medical information to your child".
The second factor was named "receptive capability of the child" and consisted of four items: "6. Your child's age is adequate to hear an explanation of medical information", "7. Your child's comprehension is adequate to hear an explanation of medical information", "16. Your child is not emotionally stressed about explanations of medical information", and "8. Your child does not have a fearful image of explanations of medical information".
The third factor was named "the child's interest and literacy regarding the explanation" and consisted of four items: "12. Your child shows interest in explanations of medical information", "13. Your child asks you questions about the content of your explanation of medical information", "10. The disease is part of your child's identity", and "11. Your child has an understanding of medical information of their disease".
The mean scores per item of the subscales of decision factors for providing disease explanations were 3.9±0.8 points, 4.1±0.9 points, and 3.4±0.9 points for the first, second, and third factors, respectively.
4. Association between Social Adaptive Skills of Children and Decision Factors for Mothers' Provision of Disease Explanations to Children with Congenital Heart Disease
The first factor was excluded from the analysis because it is associated with the mother's ability and not with the child's growth and development. The second and third factors were analyzed. The second factor was significantly associated with language skills (β=.35, p=.015) and social life skills (β=.36, p=.026), and the third factor was significantly associated with language skills (β=.41, p=.006) and daily life skills (β=.42, p=.003). In all analyses, the VIF ranged from 1.57 to 2.18 for all items, including confounders, and the Durbin-Watson ratio ranged from 1.99 to 2.30, with no multicollinearity observed. Each of these regression models was significant, with F values ranging from 2.50 to 5.06, R2 from .16 to .28 (Table 5).
DISCUSSION
We found that there were three decision factors for providing disease explanations to children with CHD by their mothers: "the mother's ability to communicate an explanation", "receptive capability of the child", and "the child's interest and literacy regarding the explanation".
The first factor reflected the mother's ability to communicate an explanation. In the first place, to provide an explanation of the illness to children, it is a prerequisite for mothers to have a sufficient understanding of the disease themselves. A previous study showed the importance of providing support to supplement the mother's eloquence by providing "auxiliary resources for explaining the disease to the child" and having nurses serve as models for the mother to explain the disease [10]. From the items comprising the first factor, it became clear that building a mother-child relationship where a disease explanation can be provided will further promote these explanations.
The items comprising the second factor suggest that mothers not only evaluate whether their children are of the appropriate age and possess the comprehension skills required to understand the explanation provided, but also whether they can adapt to negative factors, such as emotionally induced stress and fear.
The items comprising the third factor relate both to responses to explanations, such as interest and questions from the children, and children's comprehension of explanations, such as understanding and the ability to identify the disease. If children proactively engage in interest-based behavior to disease explanations, their literacy will naturally increase. Moreover, literacy leads to more interest, as children's ability to identify the disease promotes their understanding of the disease, self-management, and a desire to accept it with a positive outlook [16]. These findings suggest that interest in explanations and literacy interact with each other and that by recognizing both of these factors together, mothers might decide to explain the disease to their children. The mean scores per item for the three factors were not high. This may reflect a situation where mothers are not able to explain the disease and treatment to their children as they wish [17].
We also found that language skills were associated with the second and third factors, daily life skills were associated with the third factor, and social life skills were associated with the second factor. Language skills were associated with the second factor, "receptive capability of the child". Because of the diversity in pathology and course and the complex morphology and pathology, CHD is not easy for children to understand. Therefore, we consider that language skills, including basic language comprehension, are foundational to the understanding of the disease. Language skills were also associated with the third factor, "the child's interest and literacy regarding the explanation". The fact that language skills include a child's interest-based behavior to explanations and information, such as "asking questions orally" and "reading", as well as skills related to literacy itself, such as "understanding instructions", may also contribute to their relevance as a foundation for this factor. Furthermore, once school-aged children have acquired a certain vocabulary, they guess the meaning of new words by combining them based on their knowledge of that element, such as kanji (ideographic characters used in Japan), and create new vocabulary knowledge [18]. Additionally, if doctors use medical terms and concepts when explaining the outcomes of an examination to patients, patients may feel uncertain, and this may hinder their understanding of the disease [19]; therefore, consideration must be given to the use of disease-specific terminology in the explanation. Improving language skills based on these considerations would prepare a foundation for the "receptive capability of the child" and "the child's interest and literacy regarding the explanation", and when mothers recognize this, it would lead to active explanations of disease to their children.
Daily life skills were associated with the third factor, "the child's interest and literacy regarding the explanation." Daily life skills refer to "skills necessary for living in the home" and include "health management" as an item directly associated with diseases. In addition, children's ability to manage their disease is included in "I CAN" (interpersonal relationships and problem-solving techniques/elements acquired by children), which is one of the three elements of resilience for CHD patients in adolescence and young adulthood [20]. This suggests that children gain resilience indirectly by adapting "health management" through improving their daily life skills, which encourages them to actively engage in interest-based behavior related to disease explanations such as "shows interest in explanations of medical information" and "asks questions about the content of your explanation of medical information". Additionally, "demonstrating the ability to condition the body", which is part of health management, such as the disclosure of illness and the understanding of one's physical condition, encourages the "reconstruction of one's natural sense" [21] and the avoidance of risky behaviors (i.e., correctly exhibiting daily life skills), was also thought to be associated with gaining literacy. Therefore, "the child's interest and literacy regarding the explanation" could be enhanced by enabling children to independently take care of their personal affairs, including disease management, despite having a disease. However, the mothers of children with CHD have been reported to be less strict in their discipline than the mothers of healthy children [17], so it is necessary to conduct a collaborative assessment of the mother's views on how to approach the child's independence.
Social life skills were associated with the second factor, "receptive capability of the child". It is important for children with CHD to interact with society from an early age and for parents to create a living environment in which they can live like healthy children [22]. Among the support measures for children with CHD and their parents are "encourage your child to spend time with his/her friends as it helps him/her socialize and "join several communities, such as school, family, and friends" [23]. Therefore, children should be allowed to participate in society while adjusting to their growth and development. In school life, for example, they need to coordinate both with teachers and with other children, although they face difficulties in social participation, such as having to worry about explaining information about themselves to their friends and whether to talk about it (i.e., the "disclosure dilemma") [24]. Even upon reaching adulthood, such patients tend to have low independent consciousness, low social skills for problem-solving, and low self-confidence [25]. Therefore, there is a not-so-low barrier to social participation for children with CHD. Social life skills include "dealing with difficult situations", "group participation skills in school", and "adapting to changing environments", all of which are required to overcome these challenges. As these skills improve and the children adapt to social life, they gain a sense of self-efficacy, which in turn reduces the "emotional stress about explanations of medical information" and "fearful image of explanations of medical information", which are components of the second factor. Therefore, by improving children's social skills and supporting their adaptation to a social life that expands as they grow, the "receptive capability of the child" will improve, and mothers will be able to explain their children's diseases with confidence.
In interpersonal skills, no significant associations were shown. Children with CHD should be able to explain themselves to others, express their desire not to be treated differently, and make their own decisions regarding the scope of their activities and participation in events at school, which is their main place of life [26]. Therefore, it was predicted that children's interpersonal skills would also be associated with mothers' decision factors for providing disease explanations, but the results were contrary to this expectation. While the other three skills, such as language, daily life, and social life skills, represent children's internal skills, interpersonal skills are their external skills with others. Therefore, although interpersonal skills are essential for the social life of school-aged children, we must first focus on children's internal skills concerning the decision factors for mothers' provision of disease explanations.
In this study, the statistical analysis was conducted with a minimal sample size, so a larger-scale study is needed. The multiple regression analysis conducted in this study was aimed at removing the influence of confounding factors and examining the effect of a particular explanatory variable on the dependent variable. Therefore, the F values and R2 of the regression models were considered to be low. Moreover, in order to clarify how to provide support tailored to the specific needs of these children, it is necessary to study not only the people who provide disease explanations but also the children who receive them. In addition, since this study was conducted at a single facility, the characteristics of the facility may have been reflected in the results.
CONCLUSION
Disease explanations from mothers to their children with CHD are very important for the children to understand the disease. However, few studies have explored this topic. In this study, the following support was suggested: 1) improving language skills including technical terms to lay the foundation for "receptive capability of the child" and "the child's interest and literacy regarding the explanation"; 2) improving daily life skills to improve "the child's interest and literacy regarding the explanation"; and 3) improving social life skills to support social participation to improve "receptive capability of the child." We considered these suggestions to be important, given their novelty and significance. Clarified support is expected to be applied in clinical practice to help school-age children understand their disease and achieve appropriate development.
Notes
Authors' contribution
Conceptualization: Shinsaku Endo and Noriko Hotta; Data collection: Shinsaku Endo; Formal analysis: Shinsaku Endo and Michiyo Higuchi; Writing-original draft: Shinsaku Endo; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
This study was supported by the Japan Society for the Promotion of Science (JSPS) Grants-in-Aid for Scientific Research (Grant-in-Aid for Young Scientists B: 17K17490).
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
We are deeply grateful to all participants. We would like to express our gratitude to the doctors, and nurses for their cooperation in the survey.